Comprehensive Guide to Monitoring Blood Glucose Levels Using Structured Charts for Better Diabetes Management
This comprehensive guide explains the importance of monitoring blood glucose levels with structured charts to better manage diabetes. It covers testing timing, benefits, factors affecting levels, and how to use glucometers. Regular monitoring helps prevent complications and ensures effective treatment, making it an essential part of diabetes care for patients and healthcare providers alike.
The Importance of Regular Blood Glucose Monitoring with a Structured Chart
Maintaining optimal blood glucose levels is a cornerstone of effective diabetes management. Blood glucose, or blood sugar, refers to the amount of sugar present in your bloodstream. The body carefully regulates this concentration to ensure energy production and overall health. Glucose is the primary fuel source for your body's cells, particularly for blood cells and fat metabolism. Normal blood sugar levels fluctuate throughout the day, typically being lowest in the morning and rising after meals due to digestion and absorption processes.
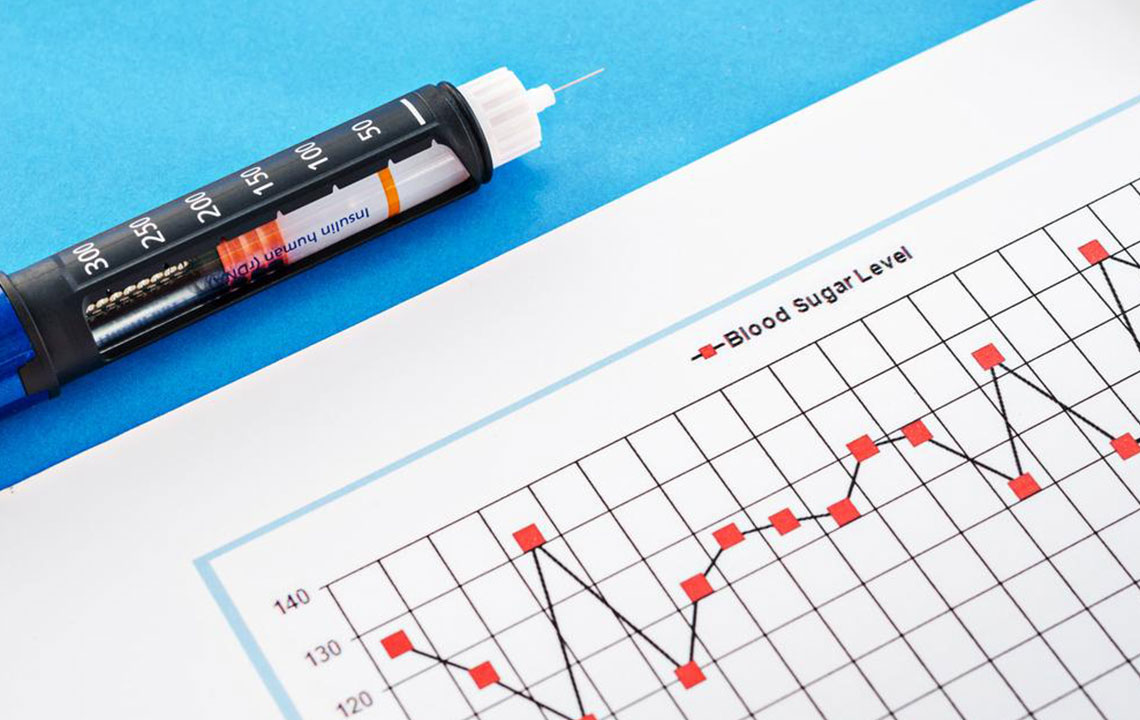
When blood glucose levels rise beyond the normal range, it signals potential health issues such as hyperglycemia, which requires timely medical attention. A well-maintained blood glucose chart serves as an essential tool for tracking these levels over time. This visual representation helps individuals and healthcare professionals understand how glucose and insulin levels vary during different times of the day and in response to specific activities. It displays peaks and drops in blood sugar, insulin, starch, and sucrose levels, providing critical insights into managing diabetes more effectively.
Using a blood glucose chart to monitor levels before and after meals offers numerous benefits that are vital for those with diabetes. This method allows for personalized management and helps prevent dangerous complications associated with uncontrolled blood sugar. Some of the key advantages include:
Assessing the effectiveness of diet, exercise, and lifestyle changes in controlling blood sugar.
Recognizing how illnesses, physical or emotional stress impact glucose levels.
Monitoring how well medications are working to keep blood sugar within target ranges.
Identifying episodes of hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar) promptly to prevent adverse health effects.
Optimal testing times: The specific timing for blood sugar testing depends on your healthcare provider's guidance and your type of diabetes. Typically, testing schedules are tailored to ensure accurate and useful data collection.
For individuals with type I diabetes, frequent testing—usually 4 to 8 times a day—is common. Testing is often recommended before meals, snacks, engaging in exercise, at bedtime, and sometimes overnight to detect fluctuations during sleep. This comprehensive data collection helps doctors adjust treatment plans effectively.
Individuals with type II diabetes may require less frequent testing, often focusing on before meals and nighttime readings if they are managing their condition with oral medications or lifestyle changes. Your doctor will personalize your testing schedule based on your unique health profile and treatment plan.
Factors influencing your blood glucose levels:
Age
Type and severity of diabetes
Duration since diagnosis
Pregnancy status, especially during gestational diabetes
Presence of complications such as nerve or kidney issues
Overall health and concurrent medical conditions
The target blood glucose levels vary depending on age and individual health circumstances. Generally, for people under 60, a normal range is approximately 80-120 mg/dL, whereas for those over 60 or with additional health issues, maintaining levels between 100-140 mg/dL is advisable. These benchmarks help reduce the risk of long-term complications associated with uncontrolled diabetes.
Monitoring blood glucose levels involves using a device called a glucometer. This small, portable electronic device requires a drop of blood, usually obtained by pricking the fingertip with a lancet. The blood sample is placed on a test strip inserted into the glucometer, which then provides a quick reading. The devices are designed for ease of use, allowing for self-testing at home once trained properly. It is crucial to record all measurements diligently, noting the date, time, medication intake, diet, physical activity, and any other relevant factors. Maintaining detailed records over time builds a comprehensive profile that helps healthcare providers optimize treatment plans and improve health outcomes.





