Comprehensive Guide to Effective Blood Sugar Monitoring for Diabetes Management
This comprehensive guide explores the importance of blood sugar monitoring in diabetes management. It covers how to use blood sugar charts, interpret readings, and their benefits in controlling blood glucose levels. Regular monitoring enables timely medical adjustments, helps prevent complications, and empowers patients. The article emphasizes practical tips for effective self-monitoring at home, making diabetes management simpler and more effective for better health outcomes.

Achieve Optimal Blood Glucose Control Through Accurate Monitoring and Charting
Diabetes mellitus is a widespread chronic disease characterized by the body's inability to regulate blood glucose levels effectively. This impairment arises either from inadequate insulin production or from the body’s resistance to insulin's effects. As a silent yet serious health threat, unmanaged diabetes significantly increases the risk of life-threatening complications such as cardiovascular diseases, nerve damage, kidney failure, blindness, and limb amputations. Consequently, maintaining precise blood sugar control is paramount for individuals living with diabetes and those at risk.
Current global statistics reveal that approximately 37% of the world's population suffers from some form of diabetes, a figure that continues to rise sharply driven by obesity, sedentary lifestyles, and poor dietary habits. As the prevalence escalates, the importance of effective blood sugar monitoring becomes even more evident for public health management and individual well-being.
Understanding Diabetes and Its Types
Diabetes is classified primarily into two main types: Type 1 and Type 2. Type 1 diabetes, also known as insulin-dependent diabetes, occurs when the immune system erroneously attacks insulin-producing cells in the pancreas, leaving individuals entirely reliant on insulin therapy. In contrast, Type 2 diabetes, which constitutes the majority of cases, involves insulin resistance and relative insulin deficiency, often associated with obesity and metabolic syndrome.
Additional forms include juvenile diabetes, which manifests early in life, and gestational diabetes that develops during pregnancy. Both conditions require specific management strategies, including lifestyle modifications and proper medication to prevent complications.
Effective management of diabetes hinges on gradual lifestyle adjustments such as balanced nutrition, regular physical activity, weight management, and adherence to prescribed medications. Regular blood sugar monitoring serves as a cornerstone in these efforts, providing real-time insights into disease control and guiding treatment modifications.
Failure to monitor and control blood glucose levels can result in dire health outcomes such as blindness, stroke, chronic infections, and in severe cases, limb amputations. These risks underscore the critical need for systematic blood sugar tracking using specialized charts and devices.
What Is a Blood Sugar Chart and How Does It Work?
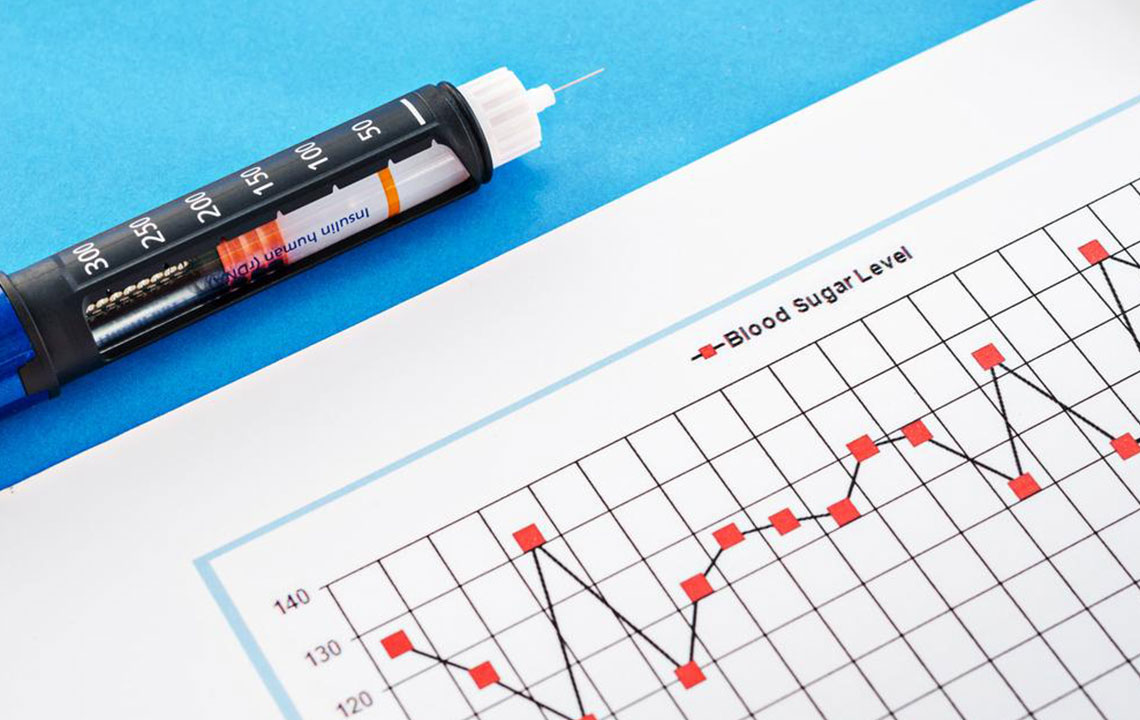
A blood sugar chart functions as a vital health tracking tool that documents fluctuations in blood glucose over time. It helps individuals and healthcare professionals understand patterns, spot anomalies, and make informed decisions about treatment plans. These charts typically record key parameters such as test dates, fasting blood glucose levels, post-meal readings, and target ranges.
Healthy fasting blood sugar levels are generally maintained between 70-130 mg/dl, whereas post-meal or random blood sugar should remain below 180 mg/dl for most individuals. Readings exceeding these thresholds may indicate deteriorating glycemic control or underlying diabetes, necessitating further clinical assessment and possible adjustments in treatment.
Conversely, dangerously low blood sugar levels below 50 mg/dl pose a risk of hypoglycemia, which can lead to confusion, loss of consciousness, and severe health consequences if not promptly addressed. Consistent use of blood sugar charts enables early detection of abnormalities, facilitating timely interventions.
Many individuals opt to download, print, or maintain digital copies of these charts for regular use, ensuring a personal record that aids in tracking long-term trends and treatment efficacy. Regular comparison of readings enables both patients and healthcare providers to evaluate whether current medications and lifestyle strategies are effective or require modification.
Practical Guidance on Using a Blood Sugar Chart Effectively
Modern blood glucose monitors come equipped with test strips that allow convenient at-home testing. By pricking the fingertip and applying a small blood sample to the test strip, individuals can receive immediate glucose level readings on the device’s display. This process is simple, quick, and typically painless, making frequent monitoring feasible.
To achieve optimal results, it’s recommended to check blood sugar levels at different times of the day, especially before and after meals, to detect any post-prandial spikes or fasting issues. Recording these values accurately in a personal chart helps identify patterns and triggers for abnormal readings, such as certain foods, activity levels, or stress.
Healthcare professionals often emphasize the importance of pre-meal (fasting) and post-meal testing to formulate accurate management strategies. Consistent monitoring supports timely insulin adjustments, dietary modifications, and lifestyle interventions, ultimately promoting better glycemic control and reducing complication risks.
The Benefits of Maintaining a Blood Sugar Monitoring Chart
While regular clinical testing is crucial, it can be costly and inconvenient. Personal blood sugar monitoring devices and charts provide an affordable, accessible alternative that encourages daily tracking. These tools are invaluable for detecting trends, preventing emergencies, and optimizing diabetes management.
Blood sugar charts interpret your mg/dl readings, offering clear insights such as identifying periods of hyperglycemia or hypoglycemia. For instance, a post-meal reading of 220 mg/dl might signal the need for medication adjustments or dietary changes to prevent complications like diabetic ketoacidosis.
Self-monitoring empowers patients by enhancing their understanding of how lifestyle factors influence their blood sugar levels. It also assists healthcare providers in fine-tuning treatment plans, evaluating medication effectiveness, and making data-driven decisions. Maintaining a consistent log simplifies communication during medical visits and supports a collaborative approach to disease management.
Besides aiding diabetics, blood sugar monitoring and charting can benefit non-diabetics as well by assessing risk factors for developing the disease, enabling early preventive measures. Early detection of abnormal patterns helps delay or prevent the onset of diabetes altogether.
In summary, the systematic use of blood sugar charts is an essential component of comprehensive diabetes control. It promotes proactive management, timely interventions, and ultimately, a higher quality of life for individuals affected by this chronic condition.