Comprehensive Insights into the Top 6 Causes of Persistent Dry Eye Syndrome
Discover the comprehensive causes of persistent dry eye syndrome. This detailed guide explores key factors such as reduced tear production, aging, medical conditions, environmental influences, and eyelid problems. Understanding these causes helps in effective management and treatment, preventing complications. Learn practical tips for prevention and when to seek professional help to maintain optimal eye health and comfort. Essential for individuals experiencing chronic dryness, this article offers insightful strategies for relief and long-term eye wellness.
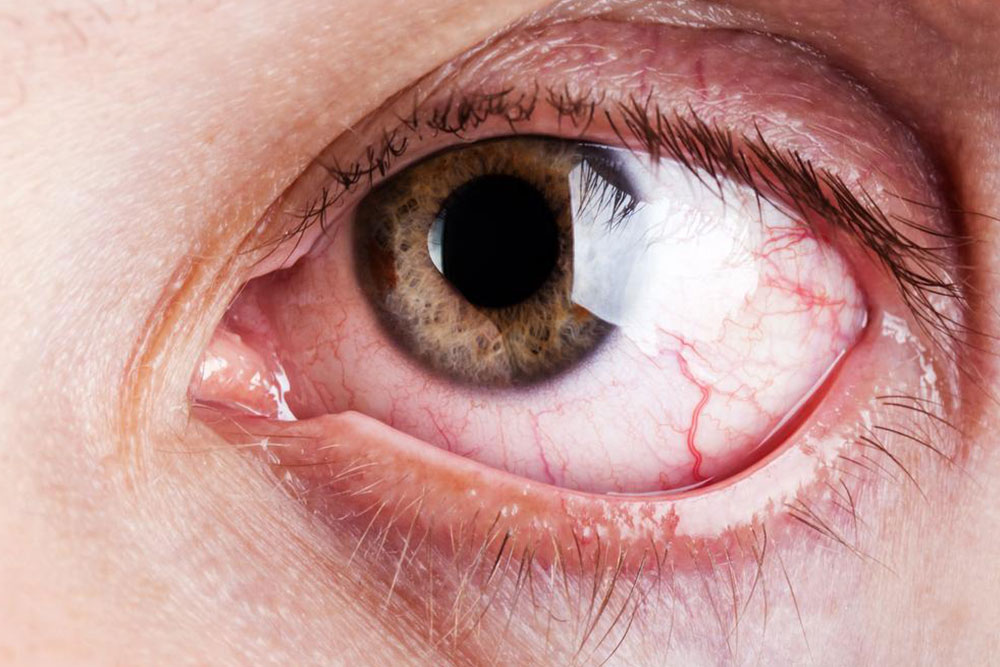
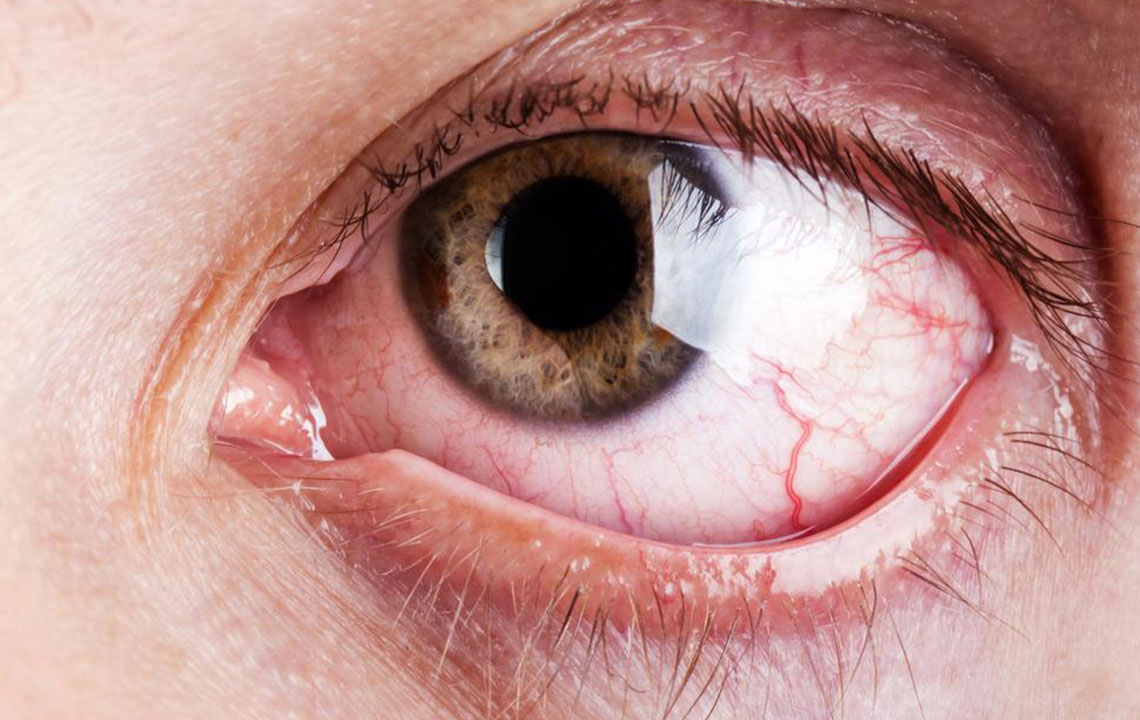
Dry eye syndrome is a prevalent ocular condition characterized by insufficient tear production or rapid tear evaporation, leading to persistent discomfort, irritation, and visual disturbances. This condition affects millions worldwide and can significantly impair quality of life if left untreated. Understanding the underlying causes of dry eye syndrome is crucial for effective management and relief. Various factors, including aging, medical conditions, environmental influences, and lifestyle choices, contribute to its development. In this comprehensive guide, we will delve into the top six causes of persistent dry eye syndrome, providing insights into each to assist individuals in recognizing symptoms and seeking appropriate treatment.
Dry eyes are more than just a nuisance; they can pose serious health risks if neglected. Chronic dry eye can lead to inflammation, damage to the corneal surface, and increased susceptibility to infections. Recognizing the primary causes helps in adopting targeted strategies for prevention and management. Let us explore these causes in detail.
1. Reduced Tear Production: The Primary Cause of Dry Eye
One of the leading causes of dry eye syndrome is decreased tear production. Tears are essential for lubricating the eyes, washing away debris, and maintaining overall ocular health. When the glands responsible for tear secretion do not produce enough tears, the eyes become dry and uncomfortable.
This condition can result from natural aging, where the lacrimal glands diminish in function. It can also be associated with specific health conditions that affect tear production. Reduced tear volume compromises the protective barrier of the eye surface, making it more vulnerable to irritation and damage.
2. Age-Related Changes and Tear Dynamics
Age significantly influences tear production. As individuals grow older, the ability of the lacrimal glands to produce sufficient tears diminishes. Studies indicate that by the age of 50, tear production declines noticeably, leading to an increased incidence of dry eye symptoms among seniors.
This decline is compounded by changes in eyelid function and blink rate, which further impair tear distribution across the ocular surface. Aging-related hormonal changes, especially in postmenopausal women, also play a role in reducing tear film stability, exacerbating dry eye symptoms.
3. Medical Conditions Contributing to Dry Eye
Several medical conditions are known to impair tear secretion or alter tear composition, resulting in dry eyes. These include:
Diabetes Mellitus: Diabetes can damage nerves that control tear production, leading to decreased tear secretion.
Autoimmune Disorders: Diseases such as Sjögren's syndrome, rheumatoid arthritis, and lupus directly affect the lacrimal glands and tear-producing cells, causing severe dryness.
Thyroid Eye Disease: Thyroid-related conditions can affect eyelid position and tear distribution, contributing to dry eyes.
Manageable through medical intervention, controlling these underlying conditions is vital in reducing dry eye severity.
4. Post-Surgical Effects: Short-Term and Long-Term Impacts
Laser eye surgeries like LASIK or cataract procedures are common corrective strategies for vision issues. However, these surgical interventions can temporarily disrupt tear production or blink dynamics, leading to dry eye symptoms.
In some cases, the disruption may persist for weeks or months post-surgery, especially if the ocular surface is irritated or if nerve endings responsible for blink reflex are affected. Adequate post-operative care, including artificial tears and protective measures, can help mitigate dry eye symptoms during recovery.
5. Environmental Factors and Lifestyle Choices
External environmental conditions play a substantial role in dry eye development. Exposure to wind, smoke, dry air, or air-conditioned environments accelerates tear evaporation and disrupts the tear film stability.
Prolonged screen time without appropriate blinking reduces tear spreading and increases dryness. Moreover, lifestyle factors such as smoking, excessive caffeine intake, contact lens wear, and insufficient hydration can exacerbate dry eye symptoms. Creating an eye-friendly environment—using humidifiers, wearing protective eyewear, and taking regular breaks during screen use—can significantly reduce the risk.
6. Eyelid Problems and Their Role in Dry Eye
Eyelid conditions, including blepharitis (inflammation of eyelid margins), eyelid malposition (ectropion or entropion), or lash abnormalities, can interfere with proper tear distribution and drainage, worsening dryness.
Particularly, dysfunction of the eyelid meibomian glands leads to abnormal oil secretion, which is essential for maintaining tear film stability. When these glands are blocked or inflamed, the tear film becomes unstable, and tears evaporate more quickly, leading to dry eyes.
Preventive Measures and When to Seek Medical Help
Recognizing these causes provides a pathway for preventive strategies. Adequate hydration, environmental modifications, blinking exercises, and proper eyelid hygiene are effective initial steps. However, persistent or severe dry eye symptoms require professional evaluation.
If discomfort, redness, or visual disturbance persists, consult an eye care specialist. Comprehensive diagnosis may include tear film assessment, eyelid examination, and identification of underlying medical conditions. Treatments can range from artificial tears and medications to lifestyle adjustments and surgical interventions if necessary.
Conclusion
Dry eye syndrome is a multifaceted condition influenced by a complex interplay of physiological, environmental, and medical factors. Its persistent form can significantly impair daily activities and overall eye health. By understanding the top six causes—reduced tear production, age-related changes, medical conditions, post-surgical effects, environmental factors, and eyelid issues—individuals can adopt effective strategies to manage symptoms and seek appropriate treatment. Maintaining good ocular hygiene, staying hydrated, protecting eyes from environmental hazards, and consulting healthcare providers for persistent issues are essential steps toward preserving eye health and comfort in the long term.