Comprehensive Guide to Managing and Treating Dry Eye Syndrome
Dry eye syndrome is a common condition affecting many adults, especially those over 40, with symptoms like irritation, redness, and blurred vision. This comprehensive guide covers causes, risk factors, symptoms, and effective treatment options, including lifestyle changes and advanced therapies like IPL. Regular eye exams and proper home care are vital for managing dry eyes and preventing serious complications. Learn how to protect your eye health and find relief from discomfort with expert-approved strategies and professional treatments tailored to your needs, ensuring healthier, more comfortable eyes.

Understanding Dry Eye Syndrome: Causes, Symptoms, and Effective Treatments
Dry eye syndrome, also known as keratoconjunctivitis sicca, is a prevalent chronic condition that impacts millions worldwide. It occurs when the eyes do not produce enough tears or when the tears evaporate too quickly, resulting in discomfort, visual disturbance, and potential damage to the eye's surface. This condition is particularly common among adults over the age of 40, but it can affect individuals of all ages, especially those with specific risk factors or underlying health issues.
Understanding the Causes and Risk Factors of Dry Eye
Dry eye syndrome develops due to a multifaceted set of causes that disrupt the eye's natural tear film. Aging is a significant factor, as tear production tends to decrease with age. Women, particularly those undergoing menopause, are more susceptible due to hormonal fluctuations that affect tear production and eye health. Environmental factors play a crucial role; exposure to dry, windy, or air-conditioned environments accelerates tear evaporation and worsens symptoms.
Extended use of contact lenses is another prominent cause. Certain medications, including antihistamines, antidepressants, and blood pressure drugs, can reduce tear production or alter tear quality. Underlying health conditions, such as autoimmune diseases like Sjogren’s syndrome, rheumatoid arthritis, thyroid disorders, and diabetes, further increase the risk of developing dry eyes. Lifestyle choices, including smoking and prolonged digital screen usage, contribute significantly, especially when combined with eyelid issues such as lagophthalmos, which impairs proper eyelid closure and protects the tears from evaporating too quickly.
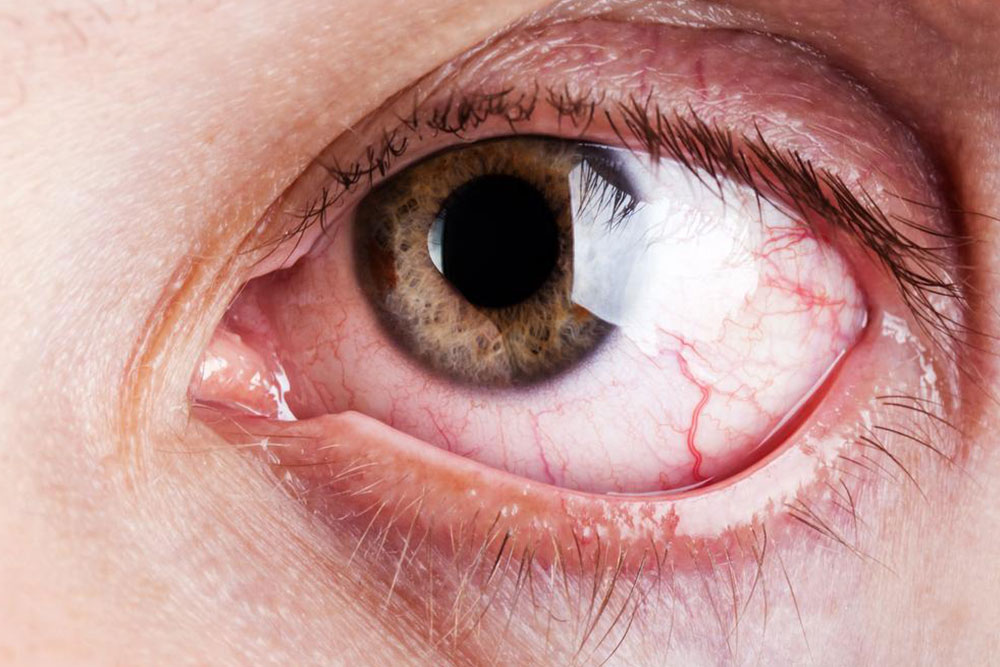
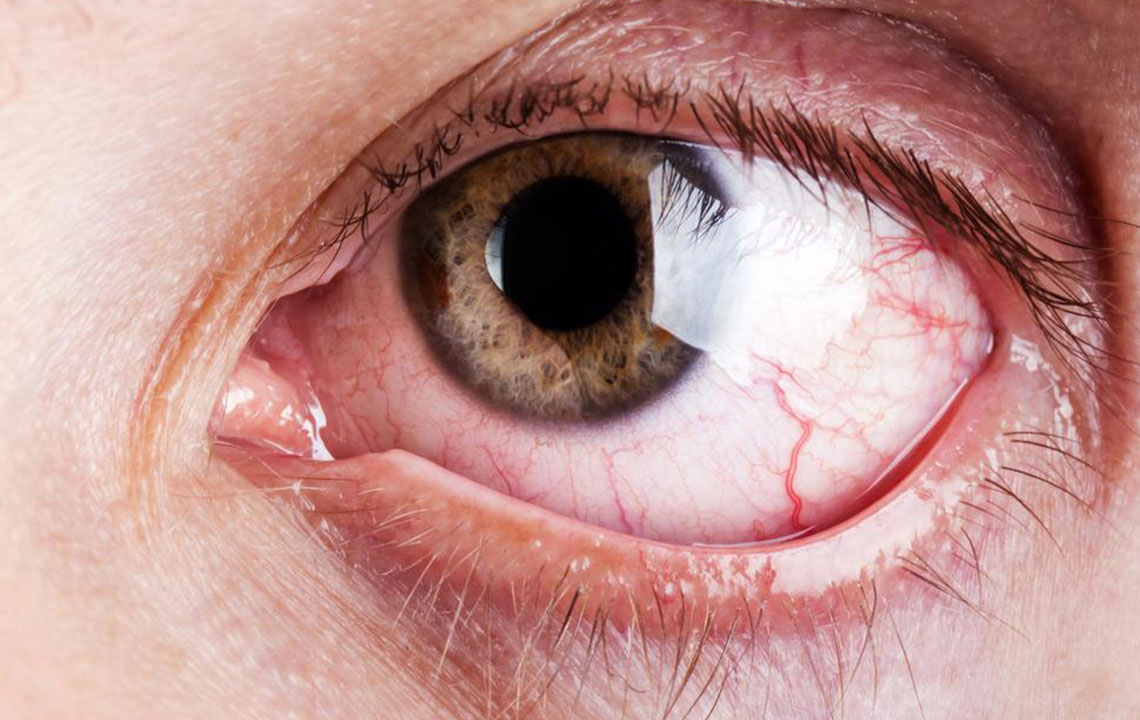
Recognizing the Symptoms of Dry Eye
The symptoms of dry eye syndrome often begin subtly but can become more severe over time. Common signs include a persistent scratchy, gritty sensation, burning, redness, and sensitivity to light. Many sufferers experience blurred vision and an unusual increase in tear production as the eyes attempt to compensate for dryness. Environmental triggers—like wind, glare, or air conditioning—can exacerbate these symptoms considerably.
Additional signs include stringy mucus around the eyes, chronic eye fatigue, and difficulty seeing clearly, especially at night. Digital device users frequently report increased discomfort after prolonged screen time, feeling the need to blink more often or experience a sensation of dryness or foreign body presence. Recognizing these symptoms early allows for prompt management, preventing potential complications such as corneal damage or conjunctivitis.
Strategies and Treatments for Managing Dry Eye Disease
Diagnosis of dry eye syndrome requires a comprehensive eye examination that measures tear quantity and quality, evaluates eyelid function, and assesses the health of the meibomian glands—small glands responsible for producing an oil layer that stabilizes the tear film. Tests such as the Schirmer test, tear breakup time, and ocular surface staining are commonly employed by eye care professionals to determine severity.
Once diagnosed, treatment strategies are tailored to individual needs. Over-the-counter artificial tears serve as the first line of defense, providing moisture and relief. In some cases, short-term corticosteroid eye drops may be prescribed to reduce inflammation. Punctal plugs, small devices inserted into tear ducts, help retain tears on the eye surface by blocking tear drainage, offering longer-lasting relief.
Warm compresses applied to the eyelids can help unblock the meibomian glands, restoring their oil secretion. Additionally, newer therapies like intense pulsed light (IPL) treatment have gained popularity for addressing lid margin inflammation and improving gland function. Regular follow-up with an eye specialist ensures optimal management and adjustment of treatments as needed.
Home Remedies and Lifestyle Adjustments to Support Eye Health
Alongside professional treatments, lifestyle modifications play a crucial role in managing dry eye symptoms. Incorporating omega-3 fatty acids into the diet—found in fish oils, flaxseeds, and walnuts—can promote healthier tear production and reduce inflammation. Maintaining good eyelid hygiene by gently cleaning eyelids with warm water and mild cleansers helps prevent clogged glands and bacterial overgrowth.
Protecting eyes from environmental stressors is essential; wearing sunglasses with UV protection reduces glare and wind exposure. Making conscious efforts to blink more frequently during screen use reduces tear evaporation, and taking regular breaks following the 20-20-20 rule (every 20 minutes, look at something 20 feet away for 20 seconds) can alleviate digital eye strain.
Furthermore, avoiding smoky or dusty environments, using humidifiers indoors, and ensuring adequate hydration support overall eye health. For contact lens users, switching to more compatible lenses or minimizing usage can lessen dryness and discomfort. Proper eyelid hygiene, such as lid massages and eyelid wipes, can also improve meibomian gland function, leading to sustained relief from dry eye symptoms.