Comprehensive Guide to Recognizing and Understanding Dry Eye Syndrome: Symptoms, Causes, and Treatments
This comprehensive guide covers the essential aspects of dry eye syndrome, including its symptoms, causes, and effective treatment options. Recognizing early signs such as irritation, blurriness, and redness can help prevent severe complications. The article explores common risk factors, from lifestyle habits to environmental influences, and offers practical management strategies like artificial tears, lifestyle modifications, and advanced therapies. With proper understanding and professional care, individuals can successfully alleviate dry eye symptoms and maintain healthy vision. Essential reading for those experiencing persistent eye discomfort.
Signs and Symptoms of Dry Eye Syndrome You Should Know
Dry eye syndrome, also known as keratoconjunctivitis sicca, is a common condition that occurs when the eyes do not produce enough tears or when tears evaporate too quickly. This leads to a persistent feeling of dryness, irritation, and discomfort that can significantly impact daily life. Understanding the signs and symptoms of dry eye syndrome is essential for early detection and effective management, preventing potential complications such as corneal damage or vision loss.
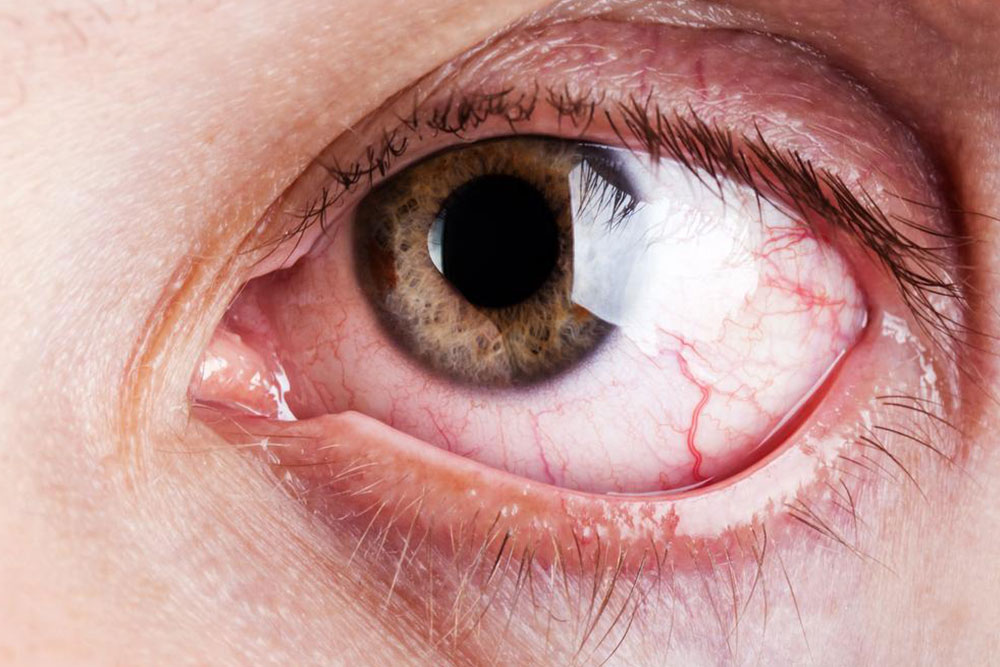
The condition manifests through various physical signs and sensations. Individuals often experience a burning or stinging feeling, which can be mild or severe depending on the degree of dryness. Many report a sensation of grit or foreign body presence in the eyes, alongside persistent redness and a tendency to blink excessively as a reflex response to irritation. Blurred vision, especially during prolonged activities like reading or working on screens, is another common symptom. These symptoms often worsen under specific conditions such as exposure to wind, dry air, or when using digital devices for extended periods.
It’s important to recognize that dry eye syndrome can cause more than just discomfort. If left untreated, it can lead to serious damage to the ocular surface. Inflammation and irritation may develop into corneal ulcers or scarring, which, in extreme cases, impair vision. Hence, early identification and treatment are crucial to preventing long-term damage. Common diagnostic signs include tear film instability, surface irregularities, and reduced tear production measured through specialized tests at eye clinics.
Several terms are associated with dry eye syndrome, reflecting its complex nature. 'Dysfunctional tear production' refers to inadequate tear secretion, often caused by gland dysfunction or hormonal imbalances. 'Keratoconjunctivitis sicca' involves inflammation of both the conjunctiva and cornea, emphasizing its inflammatory component. Recognizing these terms helps in understanding the condition's underlying issues.
Specific symptoms often observed in dry eye patients include:
Persistent eye discomfort, burning, or stinging sensations
Vision that becomes blurry at times
Redness and a sensation of heaviness or fatigue in the eyelids
String-like or mucous-like discharge from the eyes
Difficulty focusing, especially during prolonged reading or screen time
Inability to produce tears during emotional moments, such as crying
Increased sensitivity to light or wind
Understanding causes of dry eyes is equally important in managing the condition effectively. Several risk factors and underlying health issues contribute to dry eye syndrome, including lifestyle habits, environmental conditions, and systemic health problems.
Common causes encompass:
Skin conditions affecting around the eyelids, such as blepharitis, leading to dryness and inflammation
Side effects from medications like antihistamines, antidepressants, birth control pills, and drugs for Parkinson’s disease that reduce tear production
Meibomian gland dysfunction, which impairs the oil layer of tears, increasing evaporation and dryness
Allergic reactions and environmental triggers such as wind, smoke, pollution, or dry air that expedite tears’ evaporation
Vitamin deficiencies, whether excess or deficiency, impacting tear quality
Hormonal changes during pregnancy or menopause that alter tear production
Prolonged use of contact lenses, which can reduce oxygen supply and disturb tear film
Age-related changes, including conditions like arthritis, thyroid diseases, lupus, and general aging of the tear-producing glands
Infrequent blinking, common during intense screen use, which reduces tear refreshment
Addressing these factors with appropriate lifestyle adjustments and medical intervention can help manage and alleviate dry eye symptoms effectively.
Effective Treatments and Management Strategies for Dry Eye
Managing dry eye syndrome involves a combination of medical treatments and lifestyle changes. The goal is to restore tear film stability, reduce inflammation, and prevent corneal damage. Conventional treatments include the use of artificial tears, lubricating ointments, and anti-inflammatory medications prescribed by healthcare professionals.
Artificial tears are the most common first-line treatment. These over-the-counter eye drops mimic natural tears and come in various formulations to suit different needs. For acute discomfort, preservative-free options are recommended to avoid irritation from frequent use. In more severe cases, doctors may prescribe gels or ointments that provide longer-lasting lubrication, especially overnight.
Moisture-retention measures such as wearing tight-fitting, airtight goggles or wrapping around the eyes can help retain moisture and protect against environmental factors like wind or dust. These simple devices can significantly reduce tear evaporation and provide relief, especially during outdoor activities.
Innovative technologies are constantly being developed to improve dry eye management. Lipid flow devices, for instance, are designed to unblock the Meibomian glands by applying gentle heat and pressure, stimulating natural oil production. This helps restore the tear film's stability by preventing rapid evaporation. Additionally, thermal pulsation therapies are emerging as effective options for gland unrelated dry eye cases.
Anti-inflammatory treatments, such as corticosteroid eye drops or immune-modulating agents, are used in cases related to severe inflammation or autoimmune conditions. Nutritional supplements, including omega-3 fatty acids, have also shown promise in improving tear quality and reducing symptoms.
Besides medical treatments, practical steps can significantly improve comfort:
Maintain adequate humidity levels indoors using humidifiers
Take regular breaks from screens, following the 20-20-20 rule (every 20 minutes, look at something 20 feet away for at least 20 seconds)
Stay well-hydrated to ensure sufficient tear production
Manage environmental exposure by avoiding smoke and windy conditions
Prioritize eyelid hygiene to reduce inflammation and improve gland function
In summary, early diagnosis and comprehensive treatment strategies are key to managing dry eye syndrome effectively. Consulting an eye care professional for personalized assessment and tailored therapies ensures the best outcomes and helps maintain optimal eye health.