Complete Guide to Understanding and Treating Dry Eye Syndrome
This comprehensive guide explores dry eye syndrome, covering its causes, symptoms, diagnosis, and a wide range of effective treatments. It emphasizes the importance of understanding individual risk factors and adopting lifestyle changes to maintain eye health and prevent complications. With detailed insights and practical advice, readers can better manage dry eyes and improve their quality of life through informed care.

Understanding and Effectively Managing Dry Eye Syndrome
Dry eye syndrome, also known as keratoconjunctivitis sicca, is a prevalent ocular health condition that impacts millions of individuals worldwide. Characterized by insufficient lubrication and moisture on the surface of the eye, this condition can significantly impair vision and reduce quality of life. It primarily affects older adults, but it can also occur in younger populations due to various factors. Recognizing the causes, symptoms, diagnosis methods, and available treatment options is crucial for effective management and maintaining eye health.
What is Dry Eye Syndrome?
Dry eye syndrome occurs when the eyes do not produce enough tears or when the tears evaporate too quickly, leading to dryness, irritation, and discomfort. Tears play a vital role in maintaining clear vision, protecting the eyes from dust and irritants, and providing essential nutrients to the corneal surface. A disruption in tear production or tear quality can lead to inflammation, corneal damage, and persistent discomfort if not managed properly.
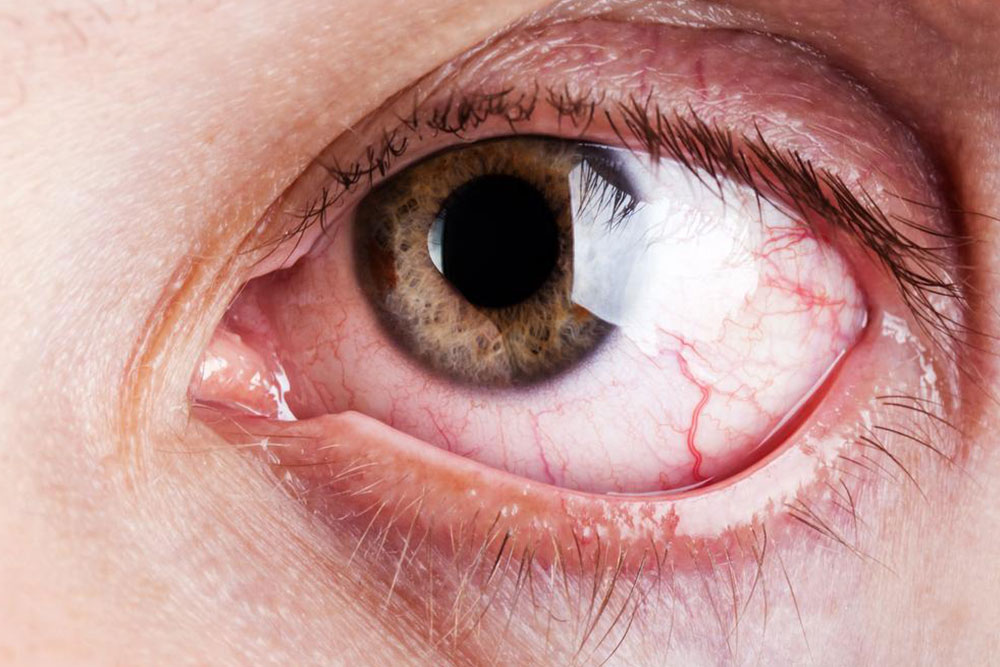
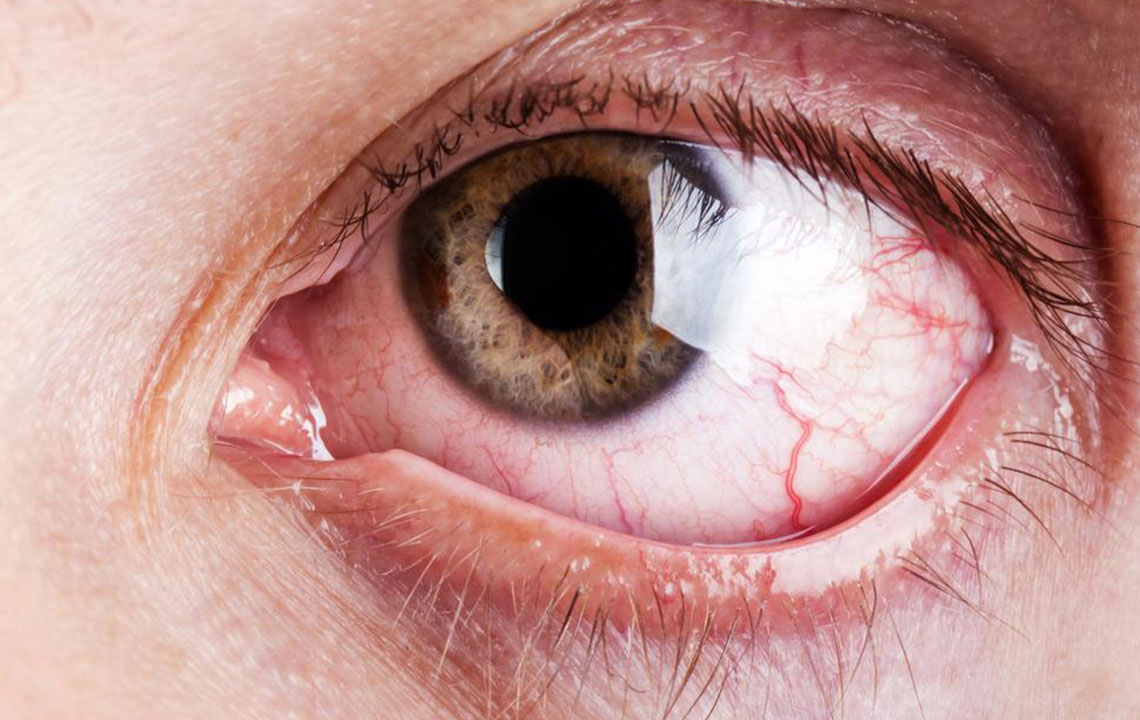
Recognizing the Symptoms of Dry Eye
Common signs and symptoms include:
Persistent eye discomfort or pain
A sensation of heaviness or a foreign body feeling in the eyes
Dryness or scratchy sensation
Redness and irritation of the conjunctiva
Blurry or fluctuating vision
Burning or stinging sensation
In some cases, reflex tearing may occur temporarily due to irritation, but this often worsens the cycle of dryness
These symptoms can affect daily activities, driving, reading, and overall comfort, prompting individuals to seek medical advice.Causes and Risk Factors for Dry Eye
Understanding the underlying causes helps in better management strategies:
Age: Tear production naturally declines as people age, notably after 65, significantly increasing the risk of dry eye syndrome.
Medications: Certain pharmaceutical drugs such as antihistamines, antihypertensives, antidepressants, and isotretinoin are known to reduce tear secretion or alter tear film stability.
Gender Influences: Women, especially during pregnancy, breastfeeding, or menopause, often experience hormonal changes that influence tear production, making them more susceptible to dry eyes.
Underlying Health Conditions: Systemic illnesses like rosacea, thyroid disorders, diabetes, and autoimmune diseases such as Sjögren’s syndrome can impair tear glands and affect tear quality.
Environmental Factors: Exposure to dust, smoke, wind, and dry air accelerates tear evaporation, worsening dryness symptoms. Extended screen time can also contribute to reduced blink rate, leading to dry, tired eyes.
Diagnosing Dry Eye Syndrome
Proper diagnosis involves comprehensive eye examinations conducted by ophthalmologists or optometrists. During assessment, healthcare providers evaluate tear quantity and quality, check for inflammation or gland dysfunction, and may perform specialized tests such as:
Schirmer’s Test: Measures tear production by placing a small strip of paper under the eyelid to see how much tear moisture is produced.
Dye Staining: Uses dyes like fluorescein or lissamine green to detect corneal damage or injury caused by dryness.
Tear Osmolarity Test: Assesses the concentration of salts in tears, indicating tear film stability and health.
Inflammation Assessment: Checks for inflammatory markers or signs of conjunctival or corneal irritation.
Proper diagnosis enables targeted treatment, potentially preventing further damage and improving patient comfort.Comprehensive Treatment Options for Dry Eye Relief
Managing dry eye syndrome involves balancing multiple approaches tailored to severity and individual needs:
Artificial Tears and Lubricating Eye Drops: Widely used for mild to moderate symptoms, these eye drops supplement natural tears, providing immediate relief and hydration.
Prescription Medications: Anti-inflammatory drugs like cyclosporine or lifitegrast help reduce ocular surface inflammation. Tear stimulants such as secretagogues may be prescribed to enhance natural tear production.
Lacrimal Plugs or Duct Occlusion Devices: Tiny biocompatible devices inserted into tear ducts block tear drainage, preserving tears on the eye surface for extended periods and alleviating dryness.
Procedural Interventions and Surgery: In cases where other treatments fail, surgical procedures such as punctal cauterization or tear duct closure may be considered to maintain ocular moisture levels.
Environmental and Lifestyle Modifications: Using humidifiers, wearing protective eyewear outdoors, reducing screen time, and practicing good eyelid hygiene can significantly decrease symptoms and prevent progression.
In addition to medical treatments, maintaining a healthy lifestyle—including staying hydrated, managing underlying health conditions, and avoiding environmental irritants—can optimize eye health and comfort.
In conclusion, dry eye syndrome is a manageable condition with proper diagnosis and personalized treatment strategies. Recognizing early symptoms and seeking professional care can prevent complications and restore visual clarity, ensuring comfort and eye health for years to come.