Comprehensive Guide to Persistent Dry Eye Syndrome and Its Management Strategies
Explore a detailed guide on persistent dry eye syndrome, including its causes, symptoms, and advanced management strategies. Learn how age, medical conditions, medications, and environmental factors contribute to chronic dryness. Discover modern treatments like artificial tears, punctal plugs, and emerging therapies that effectively alleviate symptoms and prevent complications. This comprehensive article aims to help individuals understand their condition better and seek suitable treatment options for sustained eye health and comfort.

Maintaining optimal eye health is essential for clear vision and overall well-being, and a key aspect of this is ensuring proper tear production. Tears serve a vital function by cleansing the eye surface, removing dust particles, and providing a protective barrier against environmental irritants. When the eyes do not produce enough tears, it leads to a condition known as dry eye syndrome, which can significantly impact daily life. Among these cases, persistent dry eye syndrome presents a more chronic and challenging form, where the deficiency of tears becomes a long-term issue, often requiring targeted management and treatment.
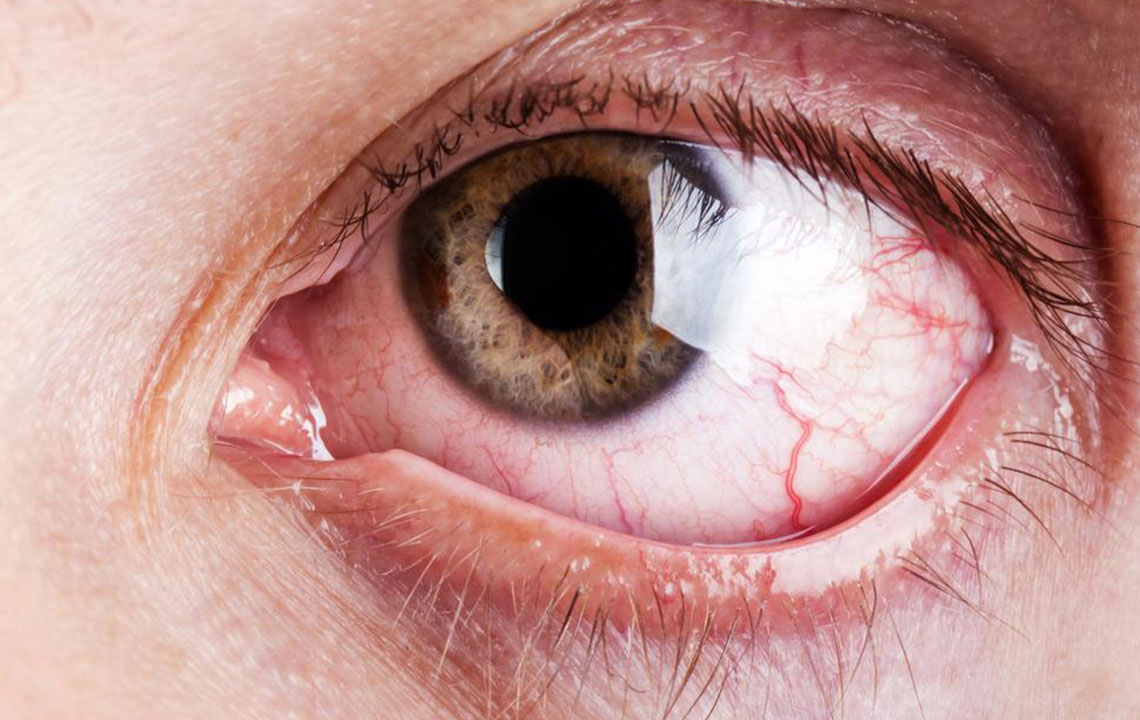
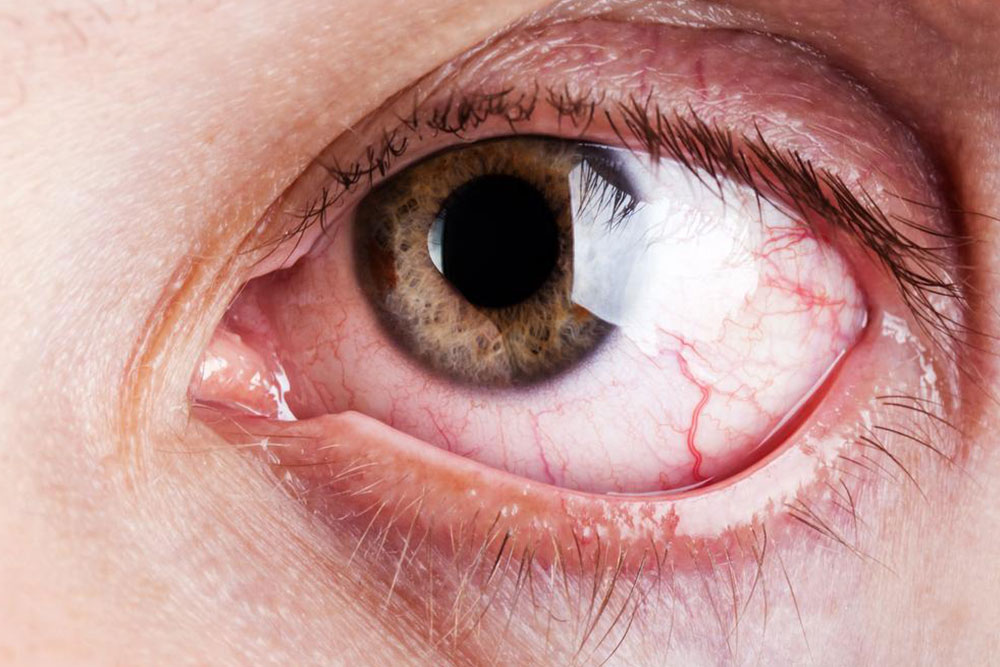
Persistent dry eye disorder, also referred to as chronic dry eye syndrome, occurs due to malfunction of the tear glands, which results in an inadequate tear film. This deficiency causes the eyes to become red, irritated, and uncomfortable, sometimes accompanied by a burning sensation or sandy feeling. In severe cases, untreated dry eye can lead to more serious complications like corneal damage or infections, highlighting the importance of early diagnosis and appropriate intervention.
The causes of persistent dry eye are diverse and often involve a combination of factors. Age plays a significant role; as we grow older, tear production naturally declines, which increases the risk of dry eye. Medical conditions such as diabetes, autoimmune diseases like Sjögren’s syndrome, and thyroid disorders can also impair tear gland function. Certain medications, including antihistamines, antidepressants, and blood pressure drugs, are known to reduce tear secretion as a side effect. Environmental factors such as exposure to wind, smoke, or dry climates intensify dryness and discomfort. Additionally, lifestyle factors, including extended screen time or inadequate blinking habits, contribute to tear film instability.
Understanding the anatomy of tear production is essential for grasping the causes of dry eye. The tear film is composed of three layers: an oily outer layer, a watery middle layer, and a mucous inner layer. The glands responsible for producing these components include the meibomian glands (which produce oils), the lacrimal glands (which secrete aqueous tears), and goblet cells (which produce mucous). Dysfunction in any of these components can destabilize the tear film, leading to dryness and irritation.
The symptoms of persistent dry eye syndrome can vary from mild discomfort to severe irritation. Common signs include redness, a gritty or sandy sensation, burning, excessive tearing (as a reflex response), blurred vision, and sensitivity to light. Some individuals may experience fluctuating symptoms that worsen throughout the day or in specific environments. Recognizing these symptoms early is crucial for effective management and to prevent further ocular surface damage.
Fortunately, there are multiple treatment options available to manage persistent dry eye effectively. The simplest and most commonly recommended are artificial tears, which can be used multiple times a day to supplement natural tear production. These eye drops help lubricate the eye surface, alleviating discomfort and protecting against environmental triggers. For more severe cases, ointments may be prescribed, providing longer-lasting relief, especially overnight.
In addition to topical treatments, medical procedures can be employed to enhance tear retention. One such procedure is temporary tear duct occlusion, which involves blocking tear drainage pathways to keep tears longer on the eye surface. More advanced options include punctal plugs — small devices inserted into tear ducts to prevent drainage, thereby increasing tear retention. These interventions are particularly useful for patients with severe or refractory dry eye symptoms.
Managing underlying causes is also a vital aspect of treatment. Adjustments in medication under supervision of healthcare providers might be necessary if drugs are contributing to dry eye. Lifestyle modifications, such as using humidifiers, taking regular breaks during screen use, and protecting eyes from wind and smoke, can significantly reduce symptoms. Additionally, maintaining proper eyelid hygiene and warm compresses can help improve meibomian gland function, restoring the natural oil layer of the tear film.
Emerging treatments and ongoing research continue to expand options for dry eye management. New formulations of lubricants, anti-inflammatory medications like cyclosporine drops, and innovations such as laser therapy are showing promising results. Patients with persistent dry eye should consult ophthalmologists or eye care specialists to develop a personalized treatment plan tailored to their specific needs, ensuring better quality of life and preservation of eye health.
In summary, persistent dry eye syndrome is a common yet complex condition that impacts millions worldwide. Recognizing its causes, symptoms, and available treatments enables timely intervention, reducing the risk of long-term damage. With advancements in medical technology and a comprehensive approach to care, managing this condition has become more effective than ever. Maintaining eye health through proper diagnosis, lifestyle adjustments, and targeted therapies can greatly improve comfort and visual clarity, helping individuals lead healthier, happier lives.