Comprehensive Guide to Insulin Pumps: Essential Knowledge for Diabetes Management
This comprehensive guide provides an in-depth understanding of insulin pumps, their components, operation, maintenance, and benefits. Designed for users and caregivers, it highlights how these devices revolutionize diabetes management by offering precise insulin delivery for better blood sugar control, increased comfort, and lifestyle flexibility.

Comprehensive Guide to Insulin Pumps: Essential Knowledge for Diabetes Management
Insulin pumps have revolutionized diabetes management by providing a seamless and efficient method of delivering insulin. These advanced, compact devices are increasingly favored by individuals living with diabetes who seek better control over their blood sugar levels and improved quality of life. In this extensive overview, we will explore the detailed aspects of insulin pumps, including their components, operational procedures, maintenance tips, and benefits. This guide aims to offer comprehensive information to patients, healthcare providers, and caregivers interested in understanding how insulin pumps function and how to optimize their use effectively.
What Are Insulin Pumps? An Introduction
Insulin pumps are small, portable electronic devices designed to mimic the way the human pancreas delivers insulin. Unlike traditional insulin injections, these devices provide continuous subcutaneous insulin infusion (CSII), giving users the flexibility to manage their diabetes more precisely. They are particularly beneficial for people with type 1 diabetes and some with type 2 diabetes who require intensive insulin therapy.
These devices deliver insulin through a streamlined system that administers either rapid-acting or short-acting insulin, precisely timed according to the user's needs. It’s important to note that long-acting insulins like Lantus or Levemir are not compatible with pump therapy because their pharmacokinetics do not suit continuous infusion. This targeted delivery helps maintain blood glucose levels within the target range, reducing the risk of fluctuations that can cause complications.
Breakdown of Insulin Pump Components
The anatomy of an insulin pump is composed of several integral parts, each playing a crucial role in the device's overall functionality:
Pump Unit: The core device, typically about the size of a credit card or smaller, contains the electronic components necessary for precise insulin delivery. It is lightweight and portable, designed for discreet use throughout the day.
Insulin Reservoir: This reservoir holds the insulin supply, which is replenished as needed. It is usually prefilled with rapid-acting insulin and can be easily replaced or refilled by the user.
Battery: Insulin pumps are powered by rechargeable or replaceable batteries that last several days, ensuring uninterrupted operation.
Microchip and Control System: The embedded microprocessor allows users to program basal rates, bolus doses, and other settings, providing precise customization tailored to individual needs.
Delivery Mechanism: A small motor or piston moves the insulin from the reservoir through tubing to the infusion site, ensuring accurate dosing.
Tubing and Infusion Set: Flexible tubing connects the pump to the infusion set attached to the patient's skin. The infusion set consists of a cannula or needle that penetrates the skin to deliver insulin subcutaneously.
Step-by-Step Operation of an Insulin Pump
Using an insulin pump correctly is essential for safe and effective diabetes management. It involves careful training and guidance from healthcare professionals. Here is an overview of the typical operational steps:
Filling the Reservoir: Start by drawing insulin from a vial or cartridge into the reservoir, taking care to eliminate air bubbles. Proper filling ensures consistent delivery and reduces the risk of complications.
Connecting the Infusion Set: Attach the infusion set securely to the filled reservoir. Activate the pump to expel any trapped air in the tubing, ensuring smooth insulin flow.
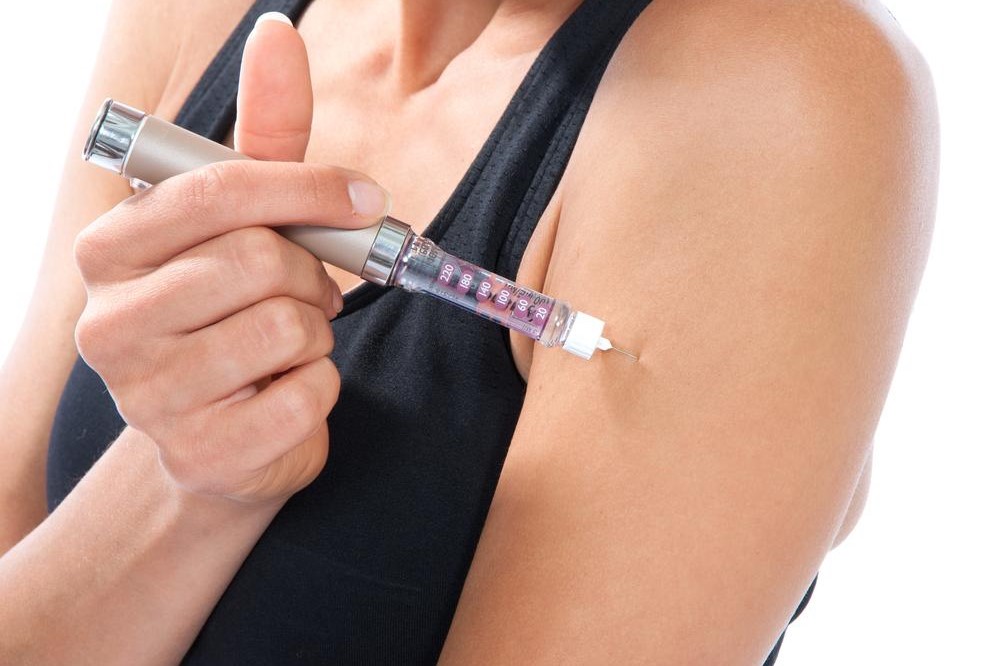
Placement of Infusion Site: Attach the infusion set to your skin at a suitable site, such as the abdomen, thighs, arms, or buttocks. It’s essential to vary infusion sites to prevent lipohypertrophy and skin irritation.
Programming the Pump: Set your basal rate (the continuous insulin delivery), bolus doses (additional doses for meals or high blood sugar readings), and other parameters based on your healthcare provider’s instructions. Regular adjustments may be necessary to optimize control.
Your healthcare team can assist with customizing settings and providing ongoing support. Remember to refill insulin and replace infusion sets every 2–3 days to maintain optimal function and hygiene practices.
Maintenance and Care of an Insulin Pump
Proper maintenance ensures the longevity and reliable performance of your insulin pump. Some key aspects include:
Refilling Insulin Reservoir: Regularly check insulin levels and refill before running low to avoid interruptions. Be cautious to prevent air bubbles that can disrupt delivery.
Changing Infusion Sets: Replace the infusion set every 2–3 days as recommended by manufacturers and healthcare providers. This practice minimizes skin irritation and infection risk.
Battery Replacement: Monitor battery life and replace batteries promptly to prevent device failure.
Cleaning and Upkeep: Follow the manufacturer’s guidelines for cleaning your pump to prevent bacterial buildup. Avoid exposing the device to extreme temperatures or water unless specified as waterproof.
Storage Tips: Store insulin at recommended temperatures. Do not use insulin directly from the refrigerator; allow it to reach room temperature to prevent air bubbles during injection.
Adhering to these maintenance practices ensures safe, reliable, and efficient use of the insulin pump, ultimately contributing to better blood glucose control and overall health outcomes.
Advantages of Using an Insulin Pump
Insulin pump therapy offers multiple benefits over traditional insulin injections, including:
More precise insulin delivery, leading to improved blood sugar control.
Reduced injection frequency, enhancing comfort and convenience.
Greater flexibility for meal timing and physical activity, promoting a normal lifestyle.
Easy adjustments for varying daily routines and carbohydrate intake.
Potential reduction in hypoglycemic episodes due to better basal rate management.
Despite their advantages, insulin pumps require consistent management and monitoring, but for many users, the improved quality of life and medical outcomes make them an indispensable part of diabetes care.
In conclusion, insulin pumps are advanced medical devices offering personalized, efficient, and flexible insulin delivery. With proper understanding, operation, and maintenance, they significantly improve diabetes management and enhance overall well-being.