Comprehensive Guide to Insulin Administration for Diabetes Management
This comprehensive guide explores various insulin administration methods for diabetes management, including traditional injections, insulin pens, pumps, and patch devices. It emphasizes the importance of personalized therapy, consistent routines, and effective blood sugar control. Designed for patients and caregivers, the article provides valuable insights into choosing the right delivery method tailored to individual needs, helping minimize complications and improve quality of life for those living with diabetes.
Comprehensive Guide to Insulin Administration for Diabetes Patients
Managing diabetes effectively requires a thorough understanding of insulin therapy, which plays a vital role in maintaining healthy blood sugar levels. Insulin therapy is essential not only for individuals diagnosed with type 1 diabetes but also for some with type 2 diabetes who may need supplemental insulin to control their condition. With a variety of insulin delivery methods and schedules available, selecting the most suitable approach is critical for effective disease management and improving quality of life. This comprehensive guide aims to provide detailed insights into insulin administration, helping patients and caregivers make informed decisions tailored to individual needs.
Insulin Management for Type 1 Diabetes
For individuals living with type 1 diabetes, insulin therapy is an indispensable aspect of daily management. These patients rely entirely on insulin since their bodies do not produce it naturally. Typically, treatment begins with multiple daily injections using syringes or insulin pens, often starting with two doses per day and adjusting based on continuous blood glucose monitoring results. The goal is to emulate natural insulin production as closely as possible, which involves timing meals, physical activity, and insulin doses carefully. Different types of insulin, including rapid-acting, short-acting, intermediate-acting, and long-acting formulations, are used in combination to achieve optimal blood sugar control, reduce complications such as stroke, nerve damage, kidney disease, and promote overall health. Consistent and precise insulin administration is critical in preventing both hyperglycemia and hypoglycemia, ensuring patients lead healthier lives despite their condition.
Insulin Therapy for Type 2 Diabetes
While type 2 diabetes patients often begin management with lifestyle modifications and oral medications, some eventually require insulin therapy to maintain blood glucose levels within a healthy range. For many, a simplified regimen, such as a single pre-bedtime injection of long-acting insulin combined with oral hypoglycemics, suffices in the early stages. However, if oral medications lose effectiveness or if blood sugar control becomes difficult, additional insulin injections may become necessary. In such cases, healthcare providers may recommend multiple daily injections or the use of insulin pumps to optimize control. The ultimate goal is to prevent complications like cardiovascular disease, nerve damage, and vision problems by maintaining stable blood glucose levels. Proper education on insulin timing, dosage, and self-monitoring is crucial for effective therapy, reducing both the physical and emotional burden of managing diabetes.
Beyond traditional injections, several innovative insulin delivery options are available, tailoring treatment to individual preferences and lifestyles. These include:
Syringe with magnifier: Designed for individuals with impaired vision, this device enhances visibility, enabling more precise injections and reducing the risk of errors.
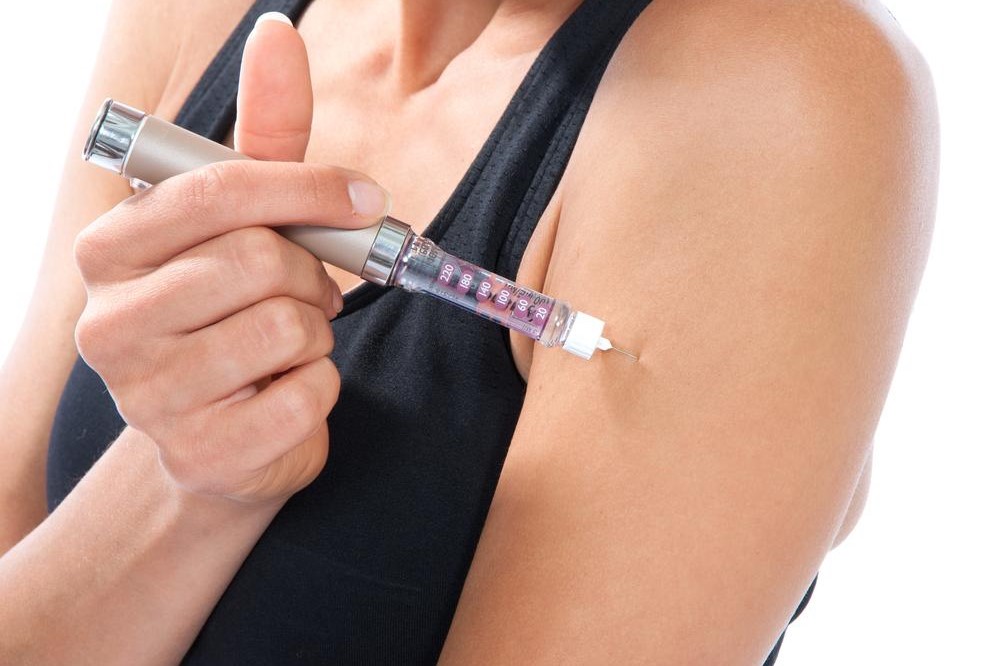
Insulin pen: A compact, easy-to-use device that resembles an EpiPen, pre-loaded with cartridges of insulin. It allows quick, painless injections with accurate dosing, making it a popular choice among patients for daily use.
Insulin pump: A sophisticated device worn on the body, often on the abdomen or thigh, that delivers continuous subcutaneous insulin through a small catheter. It is especially suitable for those needing tight glucose control or with active lifestyles, as it allows flexible dosing and better response to blood sugar fluctuations.
Patch pump: A newer, minimally invasive alternative that adheres directly to the skin and delivers insulin through a small catheter, eliminating the need for needles and tubes. This method offers convenience and discretion, encouraging consistent use among users.
Choosing the optimal insulin delivery method requires careful consultation with healthcare professionals, considering individual lifestyle, comfort, and medical needs. Proper education and training ensure that users can confidently manage their insulin therapy, maintaining stable blood sugar levels and reducing the risk of complications. With advancing technology, patients now have access to more personalized and less invasive options, empowering them to take control of their diabetes management every day.





