The Critical Importance of Neutrophils in Human Immune Defense Mechanisms
This article explores the vital role of neutrophils in immune defense, detailing their development, functions, and significance in fighting infections and autoimmune diseases. It covers causes of neutrophil deficiency and the mechanisms by which these cells eliminate pathogens, emphasizing their importance in overall health. Understanding neutrophil biology aids in advancing medical strategies to treat infections and autoimmune conditions, highlighting their critical contribution to immune system resilience.
The Essential Role of Neutrophils in Immune Function and Disease Prevention
Understanding Neutrophils: The Body’s First Line of Defense
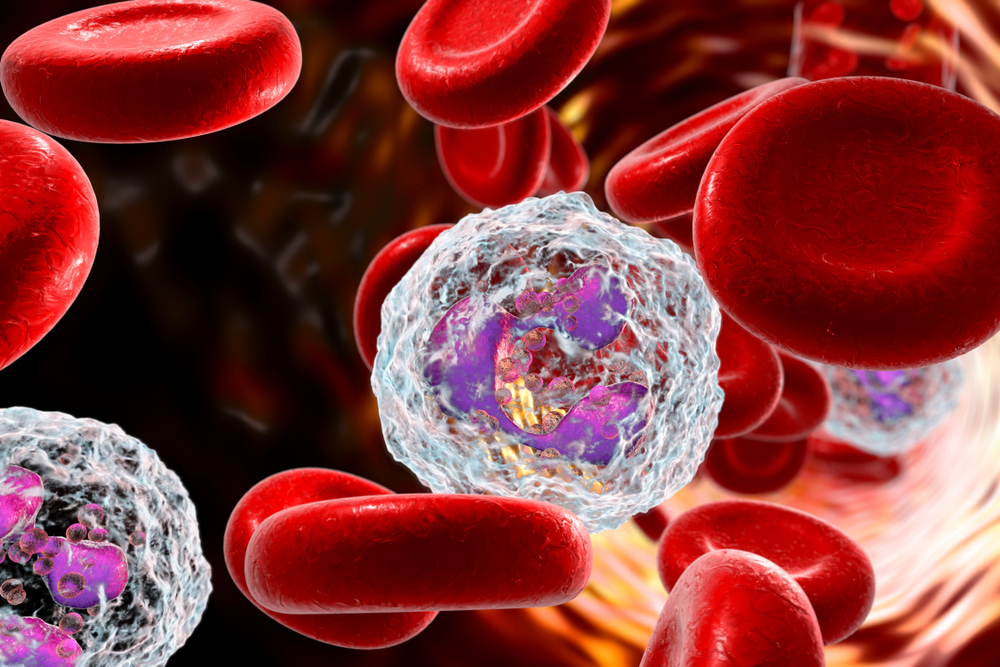
Throughout evolutionary history, multicellular organisms have developed complex defense systems to protect against invading pathogens such as bacteria, viruses, and fungi. Among these, neutrophils emerge as vital components of the immune system, acting as rapid responders to infections. These specialized white blood cells are particularly adept at identifying, engulfing, and destroying bacteria, playing an indispensable role in maintaining health. While their effectiveness against viruses is limited, neutrophils' ability to curb bacterial infections makes them essential first responders during illness.
What Are Neutrophils and How Do They Function?
Neutrophils are produced mainly in the bone marrow, specifically within the soft, spongy tissue called trabecular bone, found inside long bones such as the femur and humerus, as well as in pelvic bones.
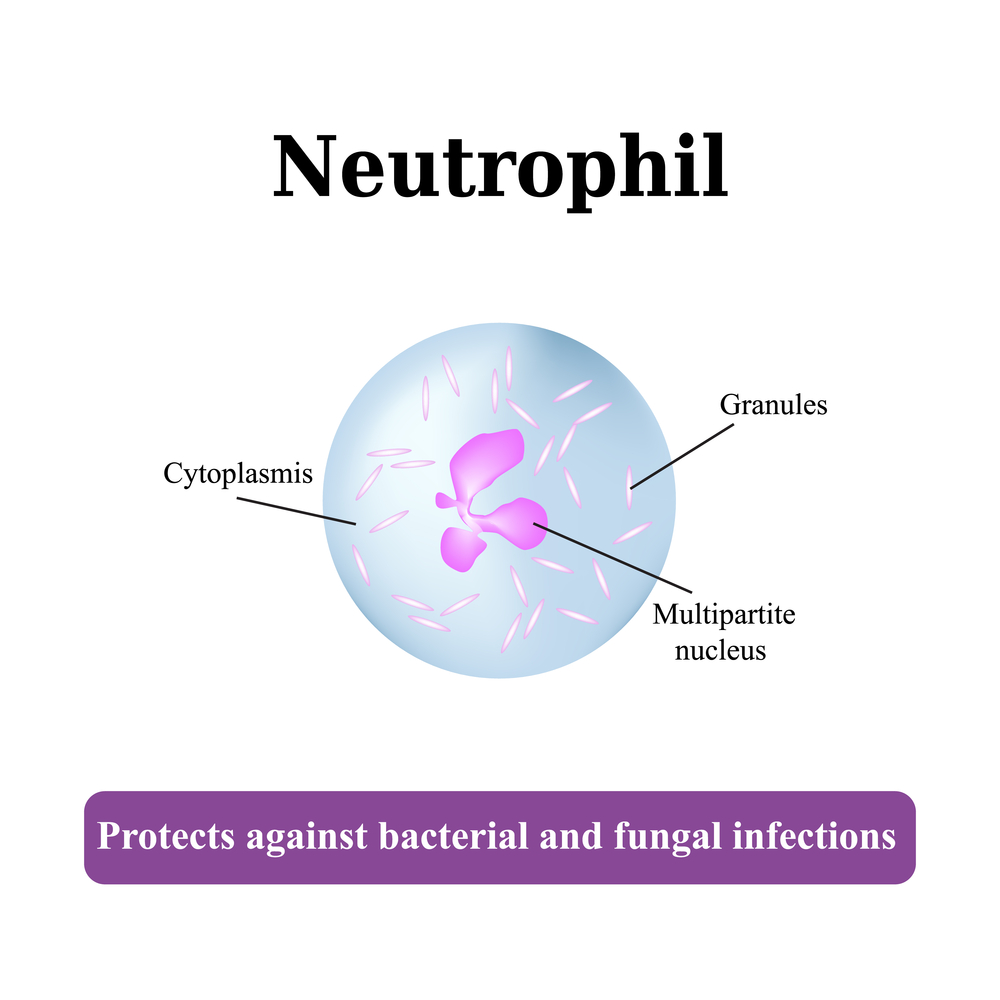
Bone marrow is the primary site for neutrophil generation, deriving them from abundant stem cell populations. These cells belong to the polymorphonuclear leukocyte family, sharing this classification with basophils and eosinophils, distinguished by their lobed nuclei and granular cytoplasm. The name 'neutrophil' reflects their characteristic staining behavior; they stain a neutral pinkish hue with standard histological dyes, aiding in their identification under microscopes.
Neutrophil Production and Normal Levels in the Bloodstream
Approximately 50% to 60% of the activity within the bone marrow is dedicated to producing neutrophils, ensuring a steady supply to meet immune needs.
In a healthy individual, circulating neutrophil counts range from roughly 40% to 70% of all white blood cells, highlighting their dominant role in immune surveillance.
Understanding Neutropenia – When Neutrophil Counts Drop
Neutropenia is a condition characterized by abnormally low levels of neutrophils, leading to increased vulnerability to infections.
Various factors, including genetic anomalies, infections, treatments, and systemic diseases, can cause reduced neutrophil counts.
Common Causes of Neutropenia
Genetic disorders such as Kostmann’s syndrome, a hereditary neutropenia, and myelokathexis, characterized by abnormal retention of neutrophils in the bone marrow.
Cancer treatments, especially chemotherapy and radiation therapy, which can destroy rapidly dividing cells like neutrophils.
Infections such as tuberculosis, hepatitis B and C, HIV/AIDS, and malaria can suppress neutrophil production or increase destruction.
Severe infections like sepsis can deplete neutrophil reserves, impairing the immune response.
Other conditions, including leukemia, hypersplenism (an overactive spleen), autoimmune diseases, and certain medications, can also lead to diminished neutrophil levels.
Functions of Neutrophils in Host Defense
Neutrophils are front-line defenders against bacterial pathogens, rapidly migrating from the bloodstream to infection sites.
The migration process, known as chemotaxis, involves sensing chemical signals released by infected tissues and responding by moving towards the source.
Neutrophils are highly motile, capable of forming pseudopodia—extensions that facilitate movement and phagocytosis.
Recent studies describe a fascinating phenomenon called neutrophil swarming, where groups of neutrophils coordinate their movement and activity to effectively contain and neutralize infections.
Mechanisms of Pathogen Elimination by Neutrophils
Once at the site of infection, neutrophils surround bacteria, extending pseudopodia to engulf and internalize pathogens—a process called phagocytosis.
Inside the neutrophil, bacteria are destroyed through a combination of reactive oxygen species and antimicrobial enzymes stored in granules.
Additionally, neutrophils can release neutrophil extracellular traps (NETs)—web-like structures composed of chromatin and antimicrobial proteins—that trap bacteria outside cells, preventing their spread and facilitating killing.
Neutrophils and Autoimmune Disorders
While neutrophils are crucial for defending against infections, their activity can sometimes cause tissue damage, especially in autoimmune diseases where the immune system erroneously targets the body’s own tissues.
Emerging research indicates that neutrophils contribute to chronic inflammation and lesion formation in conditions like atherosclerosis, where they promote the development of plaques in arterial walls.
Neutrophils can also act as sources of autoantigens, which further drive autoimmune processes, making their regulation essential for preventing immune-mediated tissue damage.
In conclusion, neutrophils are indispensable components of our immune system, providing rapid and effective defenses against bacterial infections. Understanding their development, functions, and the implications of their dysfunction opens pathways for improved treatments for infections, autoimmune diseases, and inflammatory conditions. Advances in immunology continue to reveal how these fascinating cells coordinate complex responses to maintain health and combat disease efficiently.