Comprehensive Guide to Neutrophils: Key Players in Immune Defense and Health
This comprehensive article explores the vital functions of neutrophils in the human immune system, detailing their production, mechanism of action, and clinical relevance. It provides insights into neutropenia and its causes, emphasizing the importance of maintaining healthy neutrophil levels. Ideal for anyone interested in immunology, health sciences, or medical studies, this guide enhances understanding of these essential immune cells and their role in fighting infections and supporting overall health.
Comprehensive Guide to Neutrophils: Key Players in Immune Defense and Health
Neutrophils: Essential Components of the Human Immune System
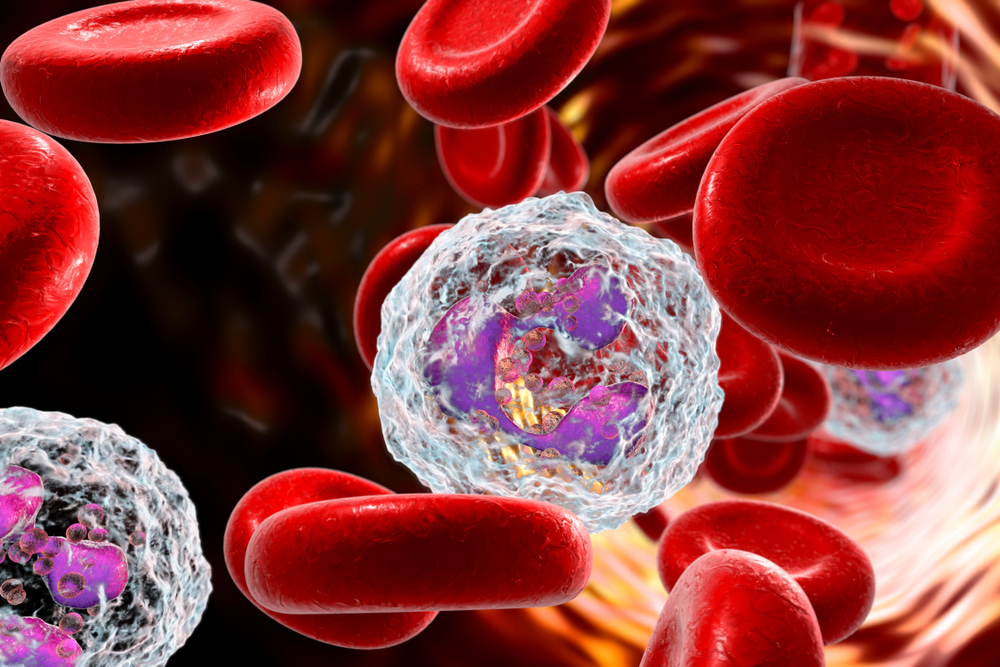
Neutrophils are a vital part of our body's innate immune defense, frequently discussed during blood tests that assess white blood cell counts. These cells are crucial in the rapid response against invading pathogens, particularly bacteria and fungi. In the complex ecosystem of blood, red blood cells (erythrocytes) dominate, responsible for oxygen transport and giving blood its characteristic red color. White blood cells, or leucocytes, though fewer in number, play vital roles in defending against infections. Among these, neutrophils are the most abundant, constituting approximately 40% to 70% of all leukocytes, making them the front-line soldiers of the immune system.
If neutrophil levels dip below their normal range, it is termed neutropenia, which can increase vulnerability to infections. Understanding how neutrophils function and where they are produced provides insights into their critical role in immune health.
Origin and Production of Neutrophils
Neutrophils are generated predominantly in the bone marrow, located within our long bones and pelvic bones, where stem cells differentiate into mature neutrophils.
Approximately 55-60% of activity in the bone marrow is dedicated to the production of neutrophils to meet the body's immune needs.
Once mature, neutrophils enter the bloodstream, where they circulate for about 5 to 90 hours before migrating into tissues, where they typically survive around 2 days.
On a daily basis, about 100 billion (10^11) neutrophils are produced, with the number rising to up to 1 trillion (10^12) during severe infections or inflammatory states.
Why Are Neutrophils So Named?
The name 'neutrophil' originates from their affinity for the neutral pink stain used in microscopy, which stains their cytoplasm.
Their production rate reflects their crucial function in combating bacterial and fungal invaders, with increased production during infections as a sign of immune response.
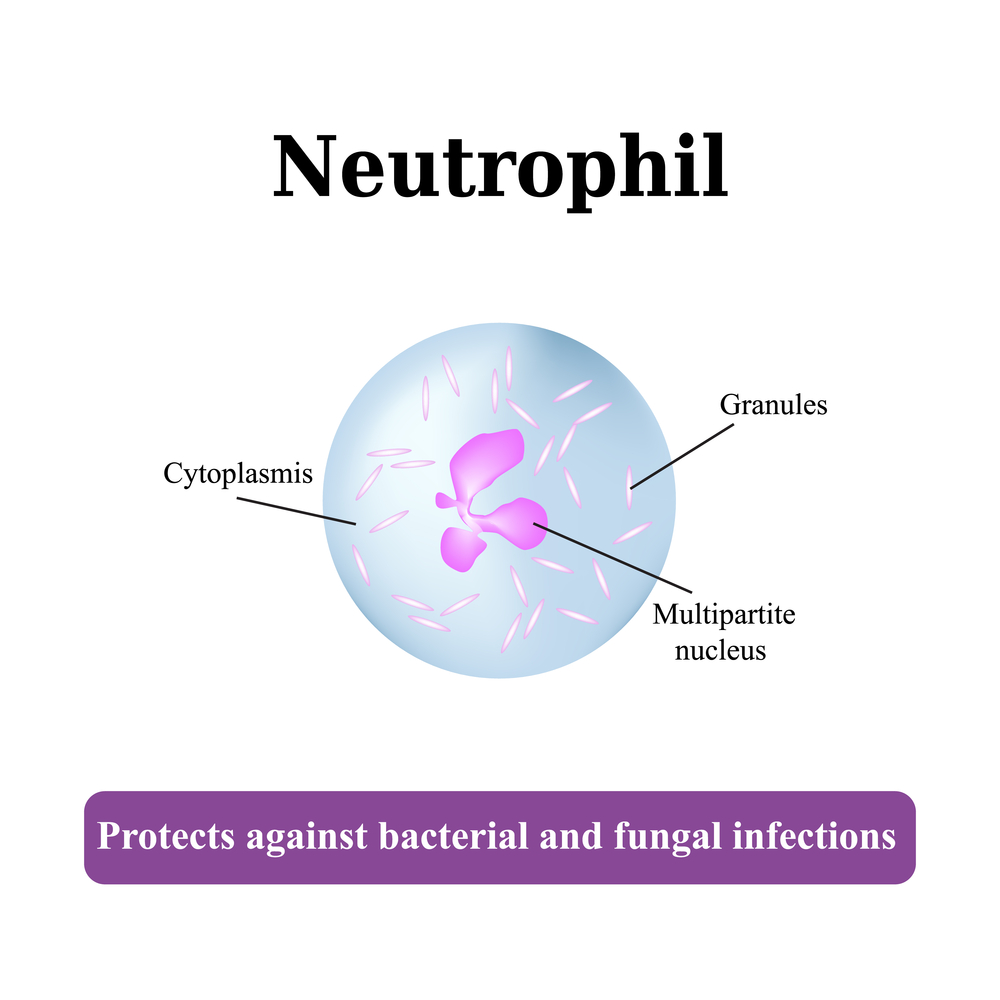
Neutrophils have a distinctive nucleus featuring 2 to 5 lobes; abnormalities like hypersegmentation can indicate health issues such as deficiencies in vitamin B12 or folic acid.
Distinctive Features of Neutrophils
Their size ranges from approximately 12 to 15 microns, but they shrink slightly when circulating in blood, down to about 9 microns.
They belong to the granulocyte family, characterized by cytoplasmic granules and a multi-lobed nucleus, sharing this group with eosinophils and basophils.
Their lobed nuclei are connected by thin chromatin strands, and as neutrophils mature, their nuclei undergo nuclear segmentation, a process unique among immune cells.
How Do Neutrophils Fight Pathogens?
Neutrophils are rapid responders that migrate swiftly from blood vessels to infection sites, a process known as chemotaxis.
They move through blood vessel walls via a process called diapedesis, extending pseudopodia—cellular projections—using specific chemical receptors to navigate toward signals from infected tissues.
This coordinated movement, dubbed neutrophil swarming, involves large groups of neutrophils converging on a single site to mount an effective attack.
At the infection site, they perform phagocytosis, engulfing bacteria and other pathogens, followed by degranulation, releasing chemicals that kill microbes.
Neutrophils also produce extracellular traps, known as NETs—net-like structures composed of chromatin and antimicrobial proteins—that effectively trap and eliminate bacteria and fungi.
Furthermore, they secrete signaling molecules that activate other immune cells, orchestrating a comprehensive immune response.
However, in autoimmune conditions, neutrophil activity can sometimes exacerbate inflammation, contributing to tissue damage.
Understanding Neutropenia
Neutropenia refers to conditions where neutrophil counts are abnormally low, increasing the risk of infections.
Common causes include chemotherapeutic treatments, radiation therapy, severe infections like hepatitis, HIV/AIDS, malaria, sepsis, and certain autoimmune disorders.
Medication side effects and hypersplenism, an enlargement of the spleen, can also contribute to decreased neutrophil levels.
Diagnosing neutropenia involves blood tests, and managing it often requires addressing the underlying cause, such as adjusting treatments or combating infections.
Overall, neutrophils are indispensable to our immune defenses, acting as the body's rapid response units against pathogens. Their production, migration, and mechanical killing mechanisms underscore the importance of maintaining healthy neutrophil levels for optimal immune function. Advances in understanding neutrophil biology continue to influence treatments for infections, inflammatory conditions, and immune disorders. Protecting and supporting neutrophil health is essential for preventing infections and maintaining overall wellness, especially in vulnerable populations undergoing medical treatments or with immune deficiencies.