Comprehensive Guide to Liver Cirrhosis: Understanding Its Stages and Management Strategies
This comprehensive article explores liver cirrhosis, detailing its stages, symptoms, potential complications, and management strategies. It emphasizes the importance of early diagnosis and lifestyle modifications to prevent progression and improve patient outcomes. Learn how different phases of cirrhosis impact health and what steps can be taken to manage this serious liver condition effectively.
Comprehensive Guide to Liver Cirrhosis: Understanding Its Stages and Management Strategies
Liver cirrhosis is a serious and progressive liver disease characterized by the replacement of healthy liver tissue with scar tissue, leading to a decline in liver function. This condition develops slowly over time and can have profound effects on overall health if not identified and managed early. The causes of liver cirrhosis are varied but commonly include chronic hepatitis infections, prolonged alcohol consumption, non-alcoholic fatty liver disease, and other chronic liver conditions. Recognizing the stages of cirrhosis is crucial for effective management and improving patient outcomes. This comprehensive guide delves into the different stages of liver cirrhosis, typical symptoms, potential complications, and the current approaches to treatment and lifestyle modifications aimed at halting or reversing disease progression.
Signs and Symptoms of Liver Cirrhosis
Persistent and unexplained fatigue
Nausea, vomiting, and unintended weight loss
Yellowing of the skin and eyes (jaundice)
Skin issues such as itching or bruising
Swelling in the abdomen (ascites) and legs
Loss of appetite and early satiety
Confusion, drowsiness, or difficulty concentrating (hepatic encephalopathy)
Understanding these symptoms can often lead to earlier diagnosis, which is vital in managing the disease effectively.
The 4 Stages of Liver Cirrhosis and Their Characteristics
Each stage of liver cirrhosis presents with distinct clinical features and risks. Knowing these stages helps healthcare providers determine the appropriate interventions and monitor disease progression.
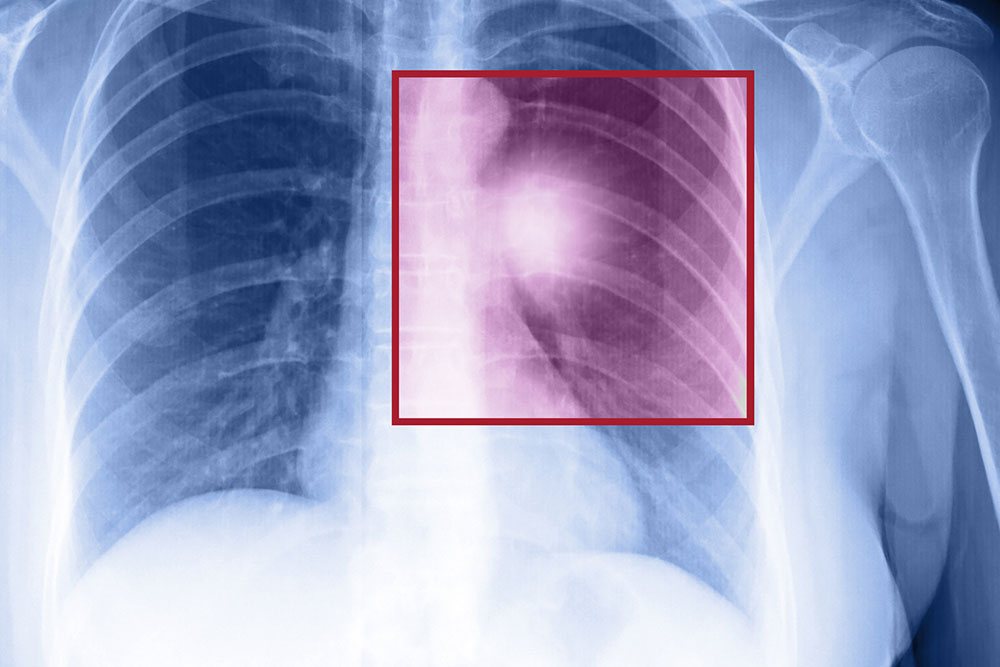
In liver cirrhosis, complications such as varices (dilated veins) and ascites (accumulation of fluid in the abdomen) are common. These issues arise due to portal hypertension, which results from impaired blood flow through the damaged liver. Understanding the various stages is crucial for predicting potential complications and planning treatment strategies.
Stage 1: Initial Damage
In the earliest phase, the liver undergoes minor inflammation and fibrosis. At this point, patients often exhibit few or no symptoms, although subtle signs like fatigue may be present. Liver function remains relatively preserved, and the risk of complications is minimal. Prompt diagnosis at this stage can allow for interventions that may slow or reverse damage, including lifestyle changes and medical treatment.
Stage 2: Moderate Fibrosis and Portal Hypertension
As fibrosis progresses, increased resistance to blood flow within the liver leads to elevated pressure in the portal vein, termed portal hypertension. This stage may present with enlarged veins (varices) in the esophagus and stomach, which hold the potential to bleed severely. Symptoms may include mild jaundice, swelling in the legs, and early signs of digestive discomfort. Early detection is critical here to prevent escalation and further liver damage.
Stage 3: Advanced Liver Damage with Ascites and Varices
In this stage, extensive scarring causes significant disruption of liver architecture and function. Patients often develop ascites, characterized by fluid accumulation in the abdomen, along with prominent varices. These conditions increase the risk of life-threatening bleeding and infections. The management may involve medications like diuretics, beta-blockers, procedures to control bleeding, and in some cases, liver transplantation becomes necessary.
Stage 4: End-Stage Liver Disease and Liver Failure
This is the most severe phase, where the liver’s ability to perform vital functions is critically compromised. Patients may experience severe complications such as uncontrollable bleeding, severe encephalopathy, and multiorgan failure. At this juncture, liver transplantation often becomes the only life-saving option. Without intervention, the prognosis is poor, emphasizing the importance of early detection and management.
Managing liver cirrhosis involves a comprehensive approach focused on slowing disease progression, preventing complications, and improving quality of life. Lifestyle changes are foundational, and include:
Strictly avoiding alcohol to reduce liver burden
Adhering to prescribed medications and vitamin supplements such as multivitamins
Limiting the use of anti-inflammatory drugs which can aggravate liver damage
Following a balanced diet that supports liver health
Regular monitoring through blood tests and imaging studies
Considering a liver transplant if the disease advances to end-stage
By understanding the stages of liver cirrhosis and adopting preventive measures, individuals can better manage their health and reduce the risk of severe complications. Early intervention remains the most effective strategy for improving prognosis and maintaining quality of life.