Comprehensive Guide to Recognizing and Managing Type 1 Diabetes Symptoms
This comprehensive guide explores the causes, symptoms, diagnosis, and management strategies for Type 1 Diabetes. It provides detailed insights into insulin therapy, injection techniques, and monitoring methods to help patients achieve optimal blood sugar control and improve quality of life. Understanding the autoimmune nature of the disease and its early signs empowers individuals to seek timely treatment and prevent serious complications.

Type 1 Diabetes Mellitus is a chronic condition that, while less common than its counterpart Type 2, accounts for approximately 5% to 10% of all diabetes cases worldwide. Generally, it manifests early in life, often before the age of 30, making it a significant concern for young adults and adolescents. Understanding the intricacies of this autoimmune disorder is essential for early diagnosis, effective management, and improving patients' quality of life.
Type 1 Diabetes is fundamentally an autoimmune disease, where the body's immune system mistakenly targets and destroys the insulin-producing beta cells in the pancreas. Insulin is a crucial hormone that facilitates the uptake of glucose into cells for energy. When beta cells are attacked and destroyed, insulin production diminishes, leading to elevated blood glucose levels. The precise causes of this immune response are not fully understood but are believed to involve a combination of genetic predisposition and environmental triggers such as viral infections or other unknown factors.
Genetic susceptibility plays a significant role, with certain genes increasing the risk of developing the disease. Environmental factors, such as exposure to specific viruses like enteroviruses, may initiate the autoimmune process in genetically predisposed individuals. This leads to the production of autoantibodies—immune proteins that mistakenly target pancreatic beta cells, further intensifying the destruction. Immune cells like CD4 and CD8 T lymphocytes are directly involved in attacking these insulin-producing cells, exacerbating the decline in insulin levels.
In the early stages of the disease, the pancreas attempts to compensate for the loss of beta cells by increasing insulin production. However, as the autoimmune destruction progresses, typically surpassing 75% of beta cell mass, insulin levels plummet. This decline results in the body's inability to regulate blood glucose effectively, leading to hyperglycemia. Symptoms often become evident during this phase and secondary complications may develop if blood sugar levels remain uncontrolled.
Recognizing the Symptoms of Type 1 Diabetes
Early detection of Type 1 Diabetes relies heavily on recognizing its hallmark symptoms, which are often quite distinctive. The most common signs include:
Frequent urination (Polyuria): Increased blood glucose levels cause the kidneys to filter out excess sugar, leading to more urine production.
Intense thirst (Polydipsia): The loss of fluids through urination results in dehydration, prompting increased water intake.
Unexplained weight loss: Despite normal or increased appetite, the body begins to break down fat and muscle for energy due to lack of insulin, leading to weight loss.
Hunger (Polyphagia): The body perceives energy deficiency due to cells not receiving glucose, triggering increased hunger signals.
Blurred vision: Elevated blood sugar levels cause osmosis, leading to fluid shifts in the eye lenses and impaired vision.
Fatigue and weakness: Cells cannot access glucose for energy, resulting in tiredness and decreased activity levels.
Increased susceptibility to infections: Elevated glucose impairs immune function, making infections more common and longer-lasting.
Nausea and abdominal pain: Sometimes, metabolic disturbances like diabetic ketoacidosis (DKA) can cause nausea, vomiting, and abdominal discomfort.
Classic Diagnostic Signs: The 3 P’s
The classic triad often used to suspect diabetes includes:
Polyuria: Excessive urination due to osmotic diuresis.
Polydipsia: Excessive thirst resulting from dehydration.
Polyphagia: Increased hunger caused by the body's inability to utilize glucose effectively.
Effective Treatment Strategies for Type 1 Diabetes
Achieving optimal management of Type 1 Diabetes necessitates lifelong insulin therapy. Since the body's ability to produce insulin is compromised, exogenous insulin administration remains the cornerstone of treatment. The goal is to mimic natural insulin secretion patterns to maintain blood glucose within target ranges, preventing complications and promoting overall health.
Insulin therapy is individualized based on factors like age, weight, lifestyle, and glucose monitoring results. Typical starting doses range from 0.4 to 1.0 units per kilogram of body weight per day. The regimen usually involves a combination of basal (long-acting) insulin to provide a steady background level and bolus (rapid-acting) insulin to manage meals and correct high blood sugar.
Types of Insulin and Administration
Various insulin formulations are available, each with specific onset and duration profiles:
Basal insulin: Long-acting insulins like insulin glargine or detemir are administered once or twice daily to control blood sugar throughout the day and night.
Bolus insulin: Rapid-acting insulins like lispro, aspart, or glulisine are taken before meals to handle the influx of carbohydrates.
Using these insulin types, the total daily dose is calculated by multiplying the patient's body weight in kilograms by the prescribed units per kg, which includes both basal and bolus requirements. Typically, around 50% of the total daily insulin dose is allocated for basal needs, with the remaining 50% divided among the meal-related bolus doses, according to carbohydrate intake.
Proper Insulin Injection Techniques and Storage
To optimize insulin absorption and minimize complications, correct injection techniques are vital. Rotating injection sites—such as the abdomen, thighs, or buttocks—helps prevent lipohypertrophy and ensures consistent absorption. Insulin should be injected at a 90-degree angle with sterile techniques, and the site should be divided into different areas to avoid tissue damage over time.
Storage of insulin is equally important. Unopened vials or pens should be stored in the refrigerator between 2°C to 8°C (36°F to 46°F). Once in use, insulin can typically be kept at room temperature for up to one month, provided it is protected from excessive heat and direct sunlight. Properly stored insulin maintains its efficacy, ensuring consistent glycemic control for the patient.
Managing Side Effects of Insulin Therapy
While insulin therapy is essential, it carries potential side effects that require management:
Hypoglycemia: Too much insulin or irregular eating can cause blood sugar to drop dangerously low, leading to symptoms like shakiness, sweating, confusion, and, in severe cases, loss of consciousness. Patients should be educated on recognizing early signs and carrying quick sources of glucose.
Weight gain: Insulin promotes fat storage; thus, careful monitoring of diet and exercise is necessary to prevent excessive weight increase.
Injection site reactions: Lipohypertrophy, skin irritation, or allergic reactions may occur. Regular site rotation and proper injection techniques mitigate these issues.
Monitoring and Follow-Up
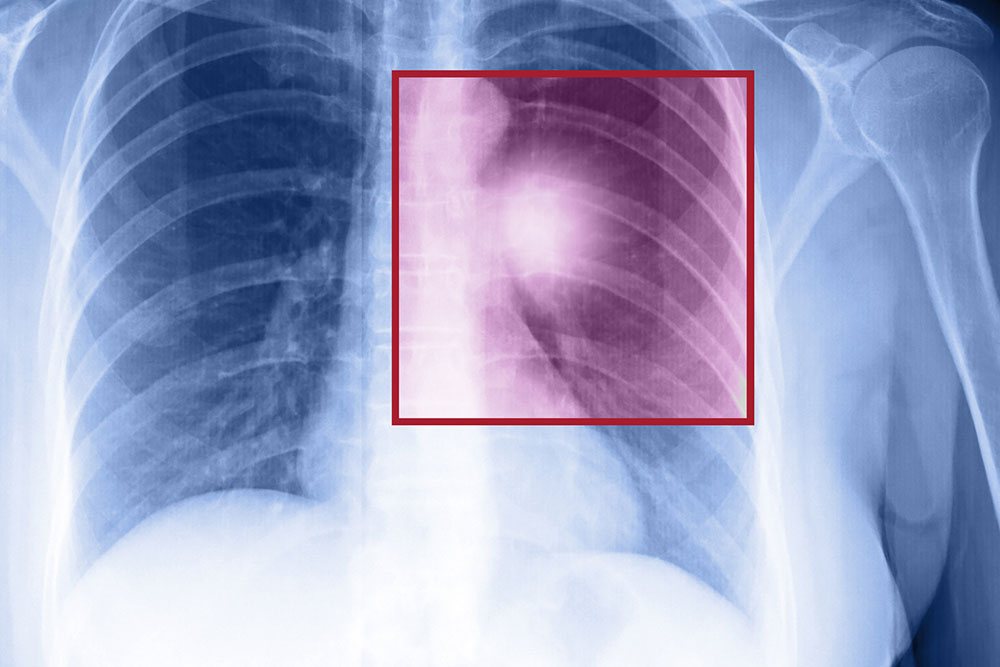
Effective management requires regular blood glucose monitoring using self-monitoring devices like glucometers or continuous glucose monitors (CGMs). This data helps patients and healthcare providers adjust insulin doses, diet, and activity levels promptly. Additionally, routine health assessments for potential complications such as neuropathy, retinopathy, kidney disease, and cardiovascular issues are vital for comprehensive care.
Conclusion
Type 1 Diabetes is a complex autoimmune disorder that demands proactive management and lifelong commitment. Understanding its symptoms, diagnosis, and treatment options empowers patients to lead healthier lives. With advancements in insulin formulations, delivery methods, and blood glucose monitoring technologies, individuals with Type 1 Diabetes can achieve excellent glycemic control and prevent long-term complications. Education, self-care, and dedicated medical support remain the pillars of successful disease management.