Comprehensive Guide to Pneumonia: Recognizing Symptoms and Exploring Effective Treatments
This comprehensive article delves into pneumonia, detailing its symptoms, causes, and the latest treatment options. It emphasizes the importance of early diagnosis and preventive measures, including vaccinations and hygiene practices, to reduce the risk of severe complications. The article also explores how pneumonia varies based on different pathogens and vulnerable populations, providing valuable insights for patients, caregivers, and healthcare professionals seeking effective management strategies.

Comprehensive Guide to Pneumonia: Recognizing Symptoms and Exploring Effective Treatments
Understanding Pneumonia: Causes, Symptoms, and Management Strategies
Pneumonia is a significant respiratory illness characterized by infection and inflammation of the lungs, primarily impacting the alveoli—the tiny air sacs within the lungs responsible for oxygen exchange. This condition can be caused by a variety of pathogens, including bacteria, fungi, viruses, and atypical organisms like mycoplasma. The infection can involve one lung or both, leading to compromised breathing and oxygen absorption. Recognizing the early signs of pneumonia is crucial, as timely treatment can significantly reduce complications and improve recovery outcomes.
Pneumonia manifests through a variety of symptoms, which can differ based on age, immune status, and the causative pathogen. Early symptoms often include a persistent cough that may produce phlegm or mucus, high fever, chills, sweating, and shortness of breath. Many patients experience chest discomfort or pain, especially when coughing or taking deep breaths. The severity of symptoms varies; children and the elderly tend to display more pronounced signs, such as rapid breathing, fatigue, or confusion.
Viral pneumonia accounts for a significant proportion of cases, primarily caused by respiratory viruses like influenza, respiratory syncytial virus (RSV), and adenoviruses. It is more common in children and older adults. These infections typically start with symptoms resembling a common cold or the flu, including wheezing, sore throat, and low-grade fever that can escalate within 12-36 hours into high fever and severe malaise.
Bacterial pneumonia, often caused by bacteria such as *Streptococcus pneumoniae*, can lead to more severe symptoms. Patients may experience extremely high fevers reaching up to 105°F, profuse sweating, bluish tint to lips and fingertips, and mental confusion, especially in vulnerable populations. Bacteria can proliferate rapidly in the alveoli, leading to pus accumulation, which further impairs lung function.
Mycoplasma pneumoniae causes an atypical form of pneumonia that generally results in milder symptoms, often with a gradual onset, affecting both children and adults. It resembles a mild bronchitis or cold but can persist longer if untreated. Fungal pneumonia, a rarer form, occurs mostly among immunocompromised individuals who have prolonged exposure to fungi in environments like soil or bird droppings. Such cases are harder to diagnose and require specialized antifungal treatments.
Hospital-acquired pneumonia, also known as nosocomial pneumonia, represents a serious health concern. It develops during hospital stays, especially among patients on ventilators (ventilator-associated pneumonia). These infections tend to involve bacteria that are resistant to multiple antibiotics, complicating treatment efforts. Aspiration pneumonia can occur when individuals inhale bacteria-laden food, drinks, or saliva due to impaired swallowing or weakened immune defenses.
Pneumonia primarily spreads through airborne droplets expelled when an infected person coughs, sneezes, or talks. Close contact with infected individuals increases the risk of transmission, emphasizing the need for good hygiene practices. Preventive measures such as wearing masks, frequent handwashing, and vaccination significantly reduce the likelihood of infection.
Effective treatment varies depending on the pathogen involved. Antibiotics like cefprozil, cefpodoxime, and cefuroxime are common options for bacterial pneumonia. Viral pneumonia may require antiviral medications, along with supportive care like rest, hydration, and oxygen therapy in severe cases. Antifungal agents are used for fungal pneumonia. It's critical for patients to complete prescribed courses of antibiotics or antivirals to prevent resistance. Additionally, managing underlying health conditions and avoiding smoking can help bolster lung health and resistance.
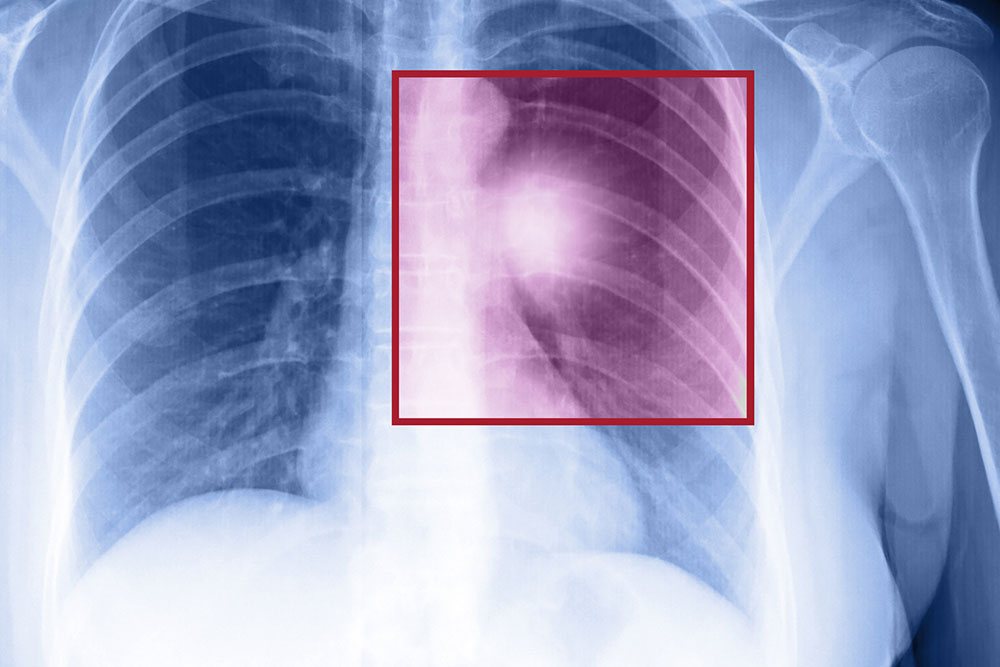
Diagnosing pneumonia involves a combination of physical examinations—listening to lung sounds with a stethoscope—and diagnostic tests such as chest X-rays, which reveal lung infiltrates or consolidation. Blood tests assess the severity and identify pathogens, while sputum and urine tests help pinpoint specific infectious agents. Advanced imaging like CT scans may be necessary to evaluate complicated cases. Recognizing high-risk groups, including children, older adults, and immunocompromised individuals, is essential for prompt diagnosis and treatment.
Prevention strategies are vital for reducing pneumonia incidence. Vaccinations against pneumococcal bacteria and influenza viruses are highly effective, especially for vulnerable populations. Maintaining good personal hygiene, avoiding exposure to known sources of infection like mold or bird droppings, and adopting a healthy lifestyle contribute to immune strength. In cases where pneumonia is diagnosed, early medical intervention is crucial to prevent complications such as lung abscesses, pleural effusion, and respiratory failure. Proper management and preventive measures can significantly improve patient outcomes and reduce hospitalization rates.