Effective Strategies and Innovative Treatments for Managing Varicose Veins
Explore effective strategies and the latest minimally invasive treatments for managing varicose veins. Learn about lifestyle modifications, surgical options, and preventive care to improve vascular health and alleviate symptoms. Early detection and professional consultation are key for optimal outcomes.

Advanced Methods for Managing and Treating Varicose Veins
Varicose veins are a common vascular condition characterized by enlarged, twisted, and swollen blood vessels that often appear beneath the skin, primarily in the legs. These veins, which typically have a bluish or purple hue, can cause discomfort, pain, and aesthetic concerns. According to research from the National Institute of Health, approximately 60% of adults worldwide are affected by varicose veins at some point in their lives. Understanding the causes, symptoms, and the latest treatment options available is essential for those seeking relief and improved quality of life.
Initially, many individuals notice the development of spider veins—tiny, web-like red or blue threads that appear on the skin's surface. These smaller veins often serve as precursors to larger, more problematic varicose veins. Factors such as sun exposure, which causes collagen breakdown, along with hormonal fluctuations, pregnancy, prolonged periods of standing or sitting, age-related changes, and weight gain, contribute to the development and worsening of these venous conditions.
Managing varicose veins involves a variety of minimally invasive surgical procedures and lifestyle adjustments, aimed at alleviating symptoms, improving appearance, and preventing complications. These treatments are designed to be performed in outpatient settings, usually without the need for hospital stays or bed rest, offering convenience and effective results for patients of different ages and health statuses.
Modern Endovenous Procedures
Sclerotherapy: This technique involves injecting a special sclerosing solution directly into the affected veins. The solution causes the veins to collapse and gradually fade within a few weeks. It is a painless procedure that does not require anesthesia, making it suitable for many patients seeking quick and effective results.
Foam Sclerotherapy: An enhanced form of sclerotherapy, where a foam version of the sclerosing agent is infused into larger veins. The foam effectively seals the vein shut, redirecting blood flow to healthier veins and reducing visible bulging.
Vein Ligation and Stripping: A surgical approach performed on an outpatient basis where problematic veins are tied off and removed through small incisions. Thanks to healthy surrounding veins, this method preserves proper blood circulation while eliminating the troublesome veins.
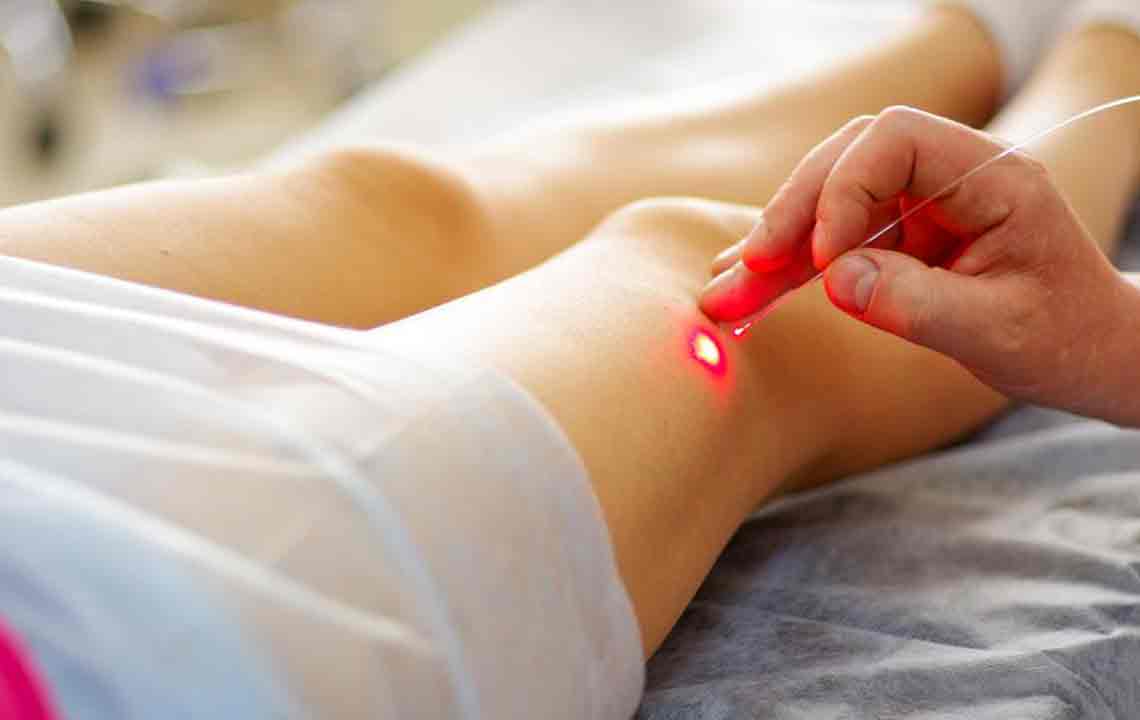
Catheter-based Techniques: Using a thin, flexible tube called a catheter, physicians apply laser or radiofrequency energy to heat and close off defective veins. As the catheter is slowly retracted, the vein collapses, and normal blood flow resumes through healthier vessels.
Endoscopic Vein Surgery: Employed in severe cases, especially when ulcers are present, this minimally invasive procedure utilizes a camera-guided device to locate the affected veins, which are then removed through tiny incisions, promoting faster healing with minimal scarring.
Laser Therapy: Highly precise laser beams target problematic veins, gradually causing them to fade without leaving scars or requiring needles. This method offers a painless alternative with quick recovery times.
Ambulatory Phlebectomy: This technique involves making small punctures in the skin to physically remove varicose veins directly. Performed under local anesthesia, it leaves no visible scars and is often used for larger veins that need removal after other treatments.
Beyond these medical procedures, lifestyle modifications play a vital role in managing and preventing the progression of varicose veins. Regular physical activities such as walking, swimming, yoga, or cycling promote healthy blood circulation and help relax the calf muscles, reducing venous pressure. Importantly, avoiding tight clothing around the waist, groin, or legs can prevent unnecessary vein constriction. Patients are advised to limit prolonged periods of standing or sitting, which can lead to increased venous pressure and vein enlargement.
Compression stockings are highly recommended as they exert gentle, steady pressure on the legs, aiding in blood flow back toward the heart. These specialized stockings come in various compression levels and should be used consistently to achieve optimal benefits. Dietary adjustments are equally important; consuming foods rich in fiber and potassium—such as oats, beans, bananas, and leafy greens—help reduce vein swelling and improve overall vascular health. Flavonoid-rich foods like apples and dark chocolate contribute to vascular flexibility and strength, further supporting vein integrity.
Early diagnosis and timely consultation with a vascular specialist or healthcare provider are crucial whenever symptoms such as leg heaviness, swelling, aching, or visible veins emerge. Addressing venous issues promptly prevents progression to more severe conditions, including ulcers, skin changes, or chronic venous insufficiency. Patients are encouraged to adopt a comprehensive approach, combining medical treatments with lifestyle modifications for optimal long-term health outcomes.
In conclusion, managing varicose veins involves a blend of minimally invasive medical procedures and proactive lifestyle changes. With advances in technology and a better understanding of venous health, individuals now have access to safer, more effective treatments that significantly improve their quality of life. If you suspect you have varicose veins or are experiencing symptoms, consult a healthcare professional to explore the best options suited to your needs and ensure a healthier, vein-healthy future.