A Comprehensive Guide to Congestive Heart Failure: Causes, Symptoms, Prevention, and Treatment
This comprehensive guide explores congestive heart failure, covering its causes, symptoms, types, risk factors, and management options. Learn how early detection and lifestyle modifications can significantly improve quality of life and prevent severe complications related to this complex cardiac condition. The article emphasizes the importance of medical treatments, healthy living, and regular check-ups for effective management and better prognosis.

An In-Depth Exploration of Congestive Heart Failure
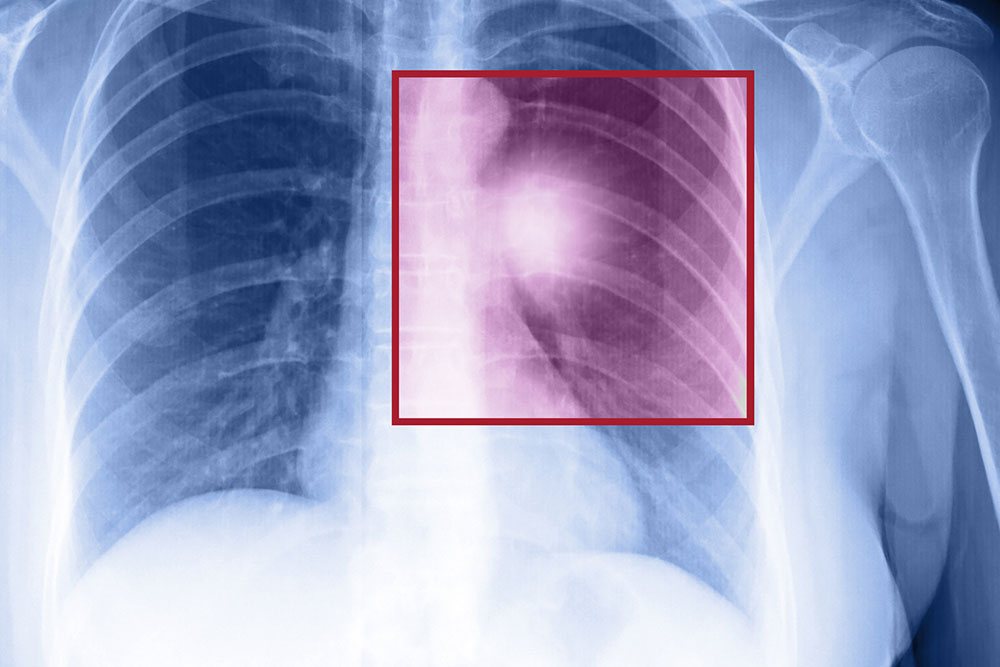
Congestive heart failure (CHF), often referred to simply as heart failure, represents a complex medical condition where the heart's ability to pump blood effectively is compromised. This impairment prevents the cardiovascular system from supplying adequate oxygen and nutrients to vital organs and tissues throughout the body. As a result, symptoms such as fluid retention, fatigue, and shortness of breath develop gradually, significantly affecting daily life and overall health. Understanding the underlying causes, recognizing early symptoms, and exploring options for management are crucial steps toward improving outcomes and maintaining quality of life.
Heart failure is a multifaceted condition with various risk factors, some of which are unavoidable due to genetics or age, while others are modifiable through lifestyle choices. Key risk factors include cardiovascular diseases like coronary artery disease, longstanding high blood pressure (hypertension), diabetes mellitus, and obesity. When multiple risk factors coexist, the likelihood of developing heart failure increases substantially. Additionally, certain lifestyle behaviors such as smoking, excessive alcohol consumption, sedentary lifestyle, and poor diet can contribute to the deterioration of cardiac function over time.
It is important to distinguish between the two main types of congestive heart failure, as their management strategies may differ:
Systolic Heart Failure (Left-Sided Heart Failure): This form occurs when the heart muscle's ability to contract forcefully is weakened, resulting in a reduced ejection fraction (the percentage of blood pumped out of the ventricles during each heartbeat). This leads to insufficient blood being circulated to meet the body's needs, causing symptoms like fatigue, shortness of breath, and fluid buildup.
Diastolic Heart Failure (Heart Failure with Preserved Ejection Fraction): In this type, the heart's ventricles become stiff and less compliant, impairing the heart's ability to fill properly during the diastolic phase. Despite normal contraction and ejection fraction, the overall blood volume pumped out is reduced, leading to similar symptoms but often different underlying causes and treatment approaches.
The progression of congestive heart failure is usually insidious, developing over months or even years. Typical early symptoms include shortness of breath (dyspnea), particularly during physical exertion or at night, which may be accompanied by episodes of waking up gasping for air (paroxysmal nocturnal dyspnea). Fluid retention manifests as swelling (edema), especially in the legs, ankles, and abdomen. Patients may experience fatigue, weakness, dizziness, and difficulty concentrating, all of which stem from inadequate blood flow and oxygen delivery.
In some cases, individuals may initially be asymptomatic, with underlying cardiac issues only detectable through medical examinations. Advanced stages of heart failure can lead to severe symptoms such as persistent coughing or wheezing, rapid or irregular heartbeat, and even fluid accumulation in the lungs (pulmonary edema), which necessitate urgent medical intervention.
Thankfully, advancements in medical therapies and a better understanding of heart failure have improved the prognosis for many patients. Management strategies encompass both pharmacological treatments and lifestyle modifications. Key medication options include ACE inhibitors, beta-blockers, diuretics, and aldosterone antagonists, which collectively help reduce the workload on the heart, control blood pressure, and alleviate symptoms.
In addition to medications, lifestyle changes are vital for effective management. Maintaining a healthy weight, following a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins, and limiting salt intake can significantly impact disease progression. Regular physical activity, tailored to individual capacity and medical advice, strengthens cardiac function and enhances overall well-being. Quitting smoking and moderating alcohol consumption are also crucial principles for reducing additional stress on the heart.
Close monitoring, routine medical check-ups, and adherence to prescribed treatments markedly improve quality of life for individuals with CHF. Advanced treatments such as implantable devices (pacemakers, defibrillators), surgical interventions, or even heart transplantation may be options for suitable candidates facing severe or refractory heart failure.
Early diagnosis and proactive management are fundamental to preventing complications and improving long-term outcomes. Anyone experiencing persistent fatigue, breathing difficulties, or unexplained swelling should seek medical evaluation promptly. With proper care, many people with congestive heart failure can lead active, meaningful lives.