Comprehensive Guide to Dry Eye Syndrome: Causes, Symptoms, and Effective Solutions
Dry eye syndrome is a prevalent eye condition characterized by insufficient tear lubrication, leading to discomfort, blurred vision, and potential eye health issues. This comprehensive guide explores the causes, symptoms, diagnosis, and various treatment options, including lifestyle changes, medications, and surgical procedures. Understanding the role of tear film layers and factors that disrupt tear stability helps patients manage their symptoms effectively. Early diagnosis and treatment are crucial for preventing complications and improving quality of life for those affected by dry eye disease.

Comprehensive Guide to Dry Eye Syndrome: Causes, Symptoms, and Effective Solutions
Dry eye syndrome, medically known as keratoconjunctivitis sicca, is a common condition that develops when the surface of the eye becomes inadequately lubricated. This impairment affects millions of individuals worldwide, especially in the United States, and can lead to significant discomfort, vision disturbances, and a decrease in quality of life. Understanding the intricacies of this condition is vital for effective management and relief.
The Importance of Tears in Eye Health
The outermost layer of the cornea depends on a delicate and dynamic system of tears to maintain proper moisture, provide nourishment, and protect against environmental hazards. Tears are not just for lubrication—they are a complex biological fluid composed of various layers and elements that keep the eye healthy and functioning optimally.
The primary role of tears is to hydrate the eye surface with each blink, ensuring clear vision by focusing light accurately onto the retina. When tear production diminishes or tear quality declines, symptoms such as dryness, irritation, and blurred vision may occur.
To better understand dry eye syndrome, it's essential to examine the composition of tears, which consist of three distinct layers:
Oil/Lipid Layer: The outermost film produced by Meibomian glands, responsible for preventing excessive evaporation of tears and maintaining surface moisture.
Aqueous Layer: The middle watery layer containing water, electrolytes, and essential proteins, primarily produced by the lacrimal glands, responsible for replenishing tears and providing essential nutrients.
Mucin Layer: The innermost layer secreted by goblet cells, which helps bind the tear film to the corneal surface and ensures even distribution of tears across the eye.
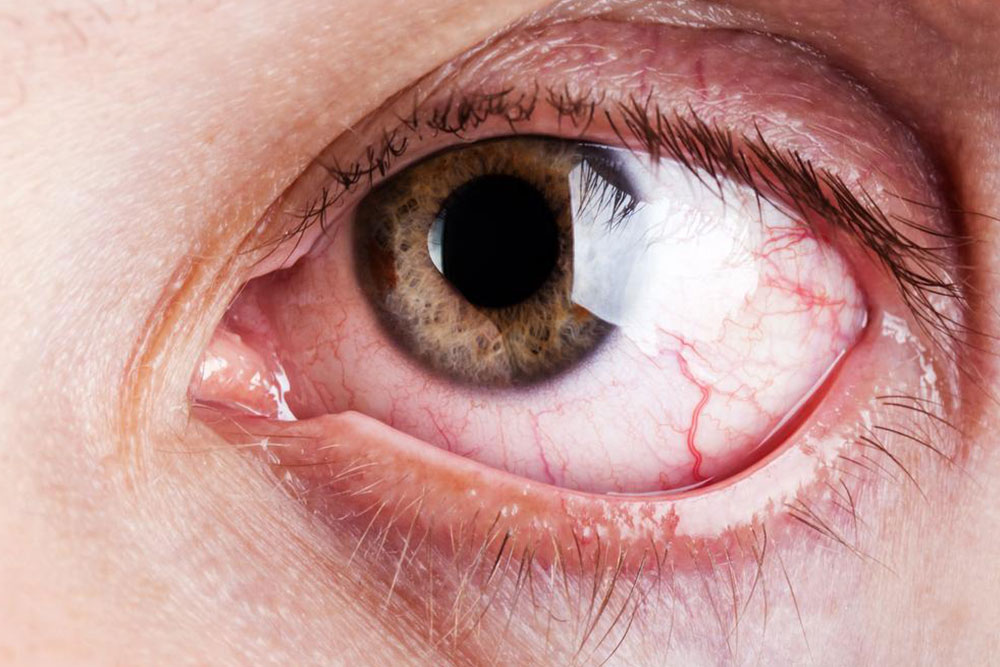
Recognizing Symptoms of Dry Eye Disease
Dry eye symptoms are frequently encountered among adults, especially women going through hormonal changes. Common signs include persistent itching, burning sensations, prickling feelings, and a sensation of dryness or heaviness in the eyes. In some cases, the eyes may produce excessive tearing initially as a reflex response, followed by dryness and irritation. Visual disturbances such as blurriness or fluctuating vision can also occur, impacting daily activities.
Underlying Causes of Dry Eyes
Dry eye syndrome results from various interconnected factors involving tear production, composition, and evaporation rates. Understanding these causes helps in selecting appropriate treatment strategies.
Medications: Certain drugs prescribed for respiratory issues, depression, or reproductive health, such as antihistamines, antidepressants, and hormonal therapies, can reduce tear production or alter tear composition.
Age-related Changes: Aging naturally diminishes tear production, with adults over 50 experiencing increased vulnerability due to glandular degeneration and hormonal fluctuations.
Inflammation: Chronic inflammation of the Meibomian glands hampers oil secretion, leading to faster tear evaporation.
Autoimmune and Systemic Conditions: Diseases like Sjögren's syndrome, rheumatoid arthritis, diabetes, and thyroid disorders significantly impair tear quality and quantity.
Hormonal Variations: Pregnancy, menopause, and hormone therapy can disrupt tear stability and increase dryness symptoms.
Environmental Factors: Exposure to wind, dust, smoke, and dry climates accelerates tear evaporation. Likewise, air conditioning and heating systems create arid environments detrimental to tear film stability.
Allergies and Eye Irritants: Allergic conjunctivitis and irritants from pollutants can worsen dry eye symptoms.
Screen Time and Visual Habits: Prolonged use of digital devices reduces blinking frequency, leading to decreased tear spread and increased surface dryness.
Post-surgical Effects: Laser eye surgeries like LASIK may temporarily disrupt tear production, causing transient dry eye symptoms during recovery.
Diagnosing Dry Eye Syndrome
If you experience persistent dry, gritty, or burning eyes, consulting an eye care professional is crucial for accurate diagnosis. The healthcare provider will perform comprehensive exams and tests such as tear film breakup time, Schirmer test, or meibography to evaluate tear stability and gland function.
Identifying any underlying health conditions or environmental factors is key to tailoring effective treatment plans.
Management and Treatment Options
Managing dry eye syndrome involves a combination of lifestyle modifications, therapeutic interventions, and sometimes medical or surgical procedures to restore tear balance and alleviate symptoms.
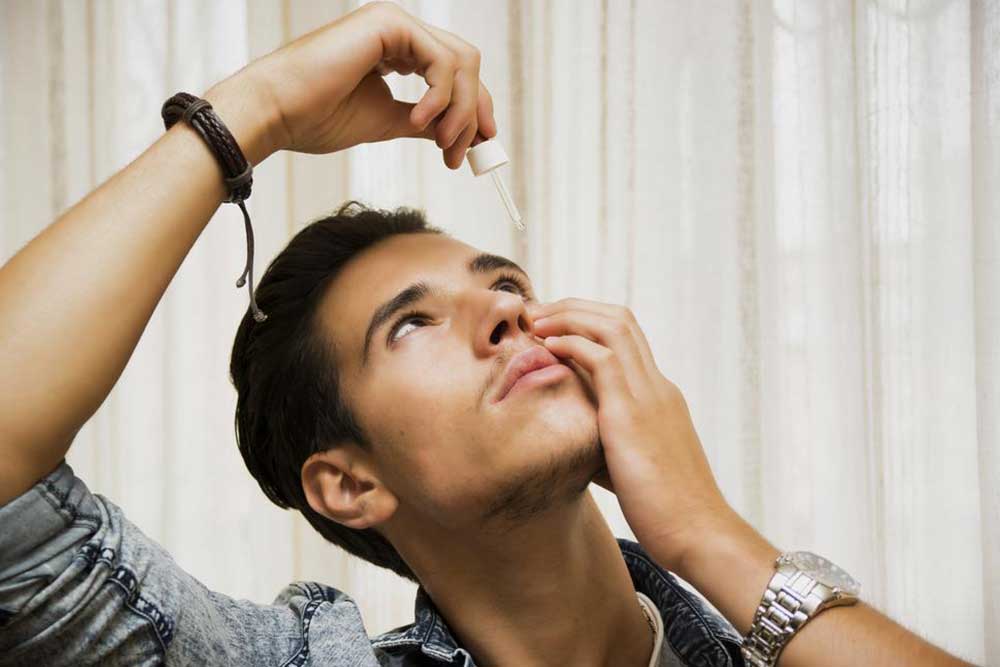
Over-the-Counter Remedies: Mild cases are often effectively managed with artificial tears, lubricating gels, or ointments that supplement natural tear production and provide immediate relief.
Environmental and Behavioral Adjustments: Wearing sunglasses outdoors, avoiding direct exposure to wind and smoke, and maintaining humidity indoors can reduce tear evaporation. Regular blinking and taking breaks during screen use help maintain tear film stability.
Climatic Modifications: Using humidifiers in dry environments and avoiding hot or dry air from heating or air conditioning systems can support eye hydration.
Medications: Prescription eye drops containing anti-inflammatory agents, cyclosporine, or lifitegrast may help reduce inflammation and improve tear production. In severe cases, oral medications or punctal plugs may be recommended.
Surgical Interventions: When conservative treatments fail, procedures such as eyelid therapy or Meibomian gland expression can help restore gland function and improve tear quality.
Emerging Therapies: Research into new treatments, including regenerative therapies and innovative drops, promises new hope for those with chronic dry eye issues.
Early intervention is essential to prevent further damage to the eye surface and to relieve discomfort. Persistent symptoms should prompt prompt consultation with eye health professionals.