Comprehensive Guide to Crohn's Disease: Symptoms, Diagnosis, and Effective Management Strategies
This comprehensive guide explores Crohn's disease, highlighting symptoms, diagnostic procedures, and management strategies. It emphasizes the importance of early detection, medical treatments, lifestyle adjustments, and ongoing research to improve patient outcomes. Learn about how to manage flare-ups effectively and enhance quality of life with expert insights into this chronic inflammatory bowel disease.

Comprehensive Guide to Crohn's Disease: Symptoms, Diagnosis, and Effective Management Strategies
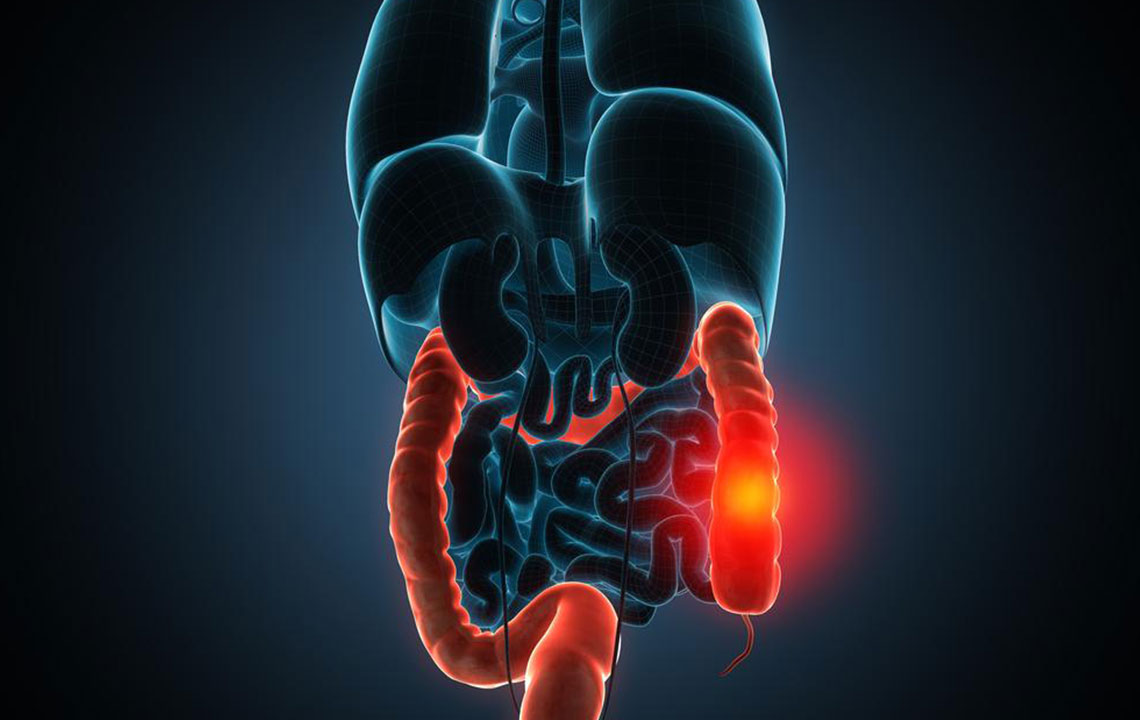
Crohn's disease is a complex, chronic inflammatory disorder that primarily affects the gastrointestinal (GI) tract. It is characterized by persistent inflammation, which can lead to swelling, ulceration, and erosion of the intestinal walls. This disease can involve any segment of the GI tract from the mouth to the anus, but it most commonly affects the terminal ileum—the last part of the small intestine—and the beginning of the colon. Given its unpredictable and relapsing nature, Crohn's disease demands comprehensive understanding and management to improve patients' quality of life.
The exact etiology of Crohn's disease remains a medical mystery. Researchers believe a combination of genetic predisposition, immune system malfunction, environmental influences, and lifestyle choices contribute to its development. An abnormal immune response triggers the body's immune system to attack healthy intestinal tissues, leading to inflammation. Factors such as smoking, stress, diet, and geographical location may influence disease onset and progression. Understanding these risk factors is essential for early detection and effective intervention.
Recognizing the symptoms of Crohn's disease is critical for timely diagnosis and treatment. Common clinical features include persistent abdominal pain, cramping, and frequent diarrhea, which may sometimes contain blood or mucus. Many patients experience unintentional weight loss, persistent fatigue, and fever, particularly during flare-ups. Additional complications can include mouth sores, anal fissures, fistulas, and joint pains, which reflect the systemic nature of the disease. A family history of inflammatory bowel disease (IBD) significantly increases the risk, and smoking is known to exacerbate symptoms and disease severity.
Diagnosis of Crohn’s disease involves a multifaceted approach. Physicians utilize physical examinations, detailed medical histories, and laboratory tests, such as complete blood counts (CBC) to detect anemia or infections. Blood tests also evaluate markers of inflammation like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). Stool analysis helps rule out infections and detect bleeding. Endoscopic procedures, primarily colonoscopies, allow direct visualization of inflamed areas and enable biopsies for histopathological examination, which confirm inflammatory changes characteristic of Crohn's disease. Additionally, advanced imaging techniques such as computed tomography (CT) scans, magnetic resonance imaging (MRI), and capsule endoscopy provide detailed views of the intestines and help assess disease extent and complications.
The primary aim of Crohn's disease treatment is to reduce inflammation, manage symptoms, and prevent disease complications. Medications play a crucial role in controlling flare-ups and maintaining remission. Commonly prescribed drugs include aminosalicylates for mild to moderate cases, corticosteroids for short-term acute management, immunosuppressants, biologic agents (such as anti-TNF therapies), and antibiotics to combat infections or reduce bacterial overgrowth. Severe cases may require surgical procedures like resection of diseased intestinal segments, especially when complications such as strictures, fistulas, or abscesses occur. Surgery is typically considered after exhausting medical treatments, and while it can provide symptom relief, it does not cure the disease, which may recur post-operation.
Beyond medications and surgeries, holistic management strategies are vital for enhancing patient well-being. Nutritional support is fundamental; many patients benefit from tailored diets including liquid nutrition, high-protein, calorie-dense foods, and specific dietary modifications to minimize symptoms. Nutritional deficiencies common in Crohn's disease—such as vitamin B12, vitamin D, iron, and zinc—require supplementation. Lifestyle adjustments, like quitting smoking, stress management, and regular exercise, contribute significantly to disease control. Complementary therapies, including massage, acupuncture, or herbal supplements such as ginseng, are often used to improve overall quality of life, although their efficacy varies among individuals. Regular monitoring and follow-up with healthcare providers are essential for optimal disease management and early detection of potential complications.
Living with Crohn’s disease is a continuous journey of managing symptoms and preventing flare-ups. Advances in medical research are ongoing, with new biologic drugs and personalized treatment plans offering hope for better disease control. Patient education about disease mechanisms, medication adherence, and lifestyle modifications remains a cornerstone of effective management. While a cure for Crohn's disease has yet to be discovered, diligent medical care and lifestyle changes can help patients lead active, fulfilling lives despite the challenges posed by this autoimmune disorder.