Comprehensive Guide to Recognizing and Managing Diverticulitis Symptoms
This comprehensive guide provides detailed information on recognizing the symptoms of diverticulitis, its causes, diagnostic procedures, and management strategies. Emphasizing the importance of early detection and lifestyle modifications, it aims to educate readers on how to prevent and effectively treat this common intestinal condition. The article is suitable for those interested in health and wellness, especially older adults or individuals with digestive health concerns seeking in-depth knowledge about diverticulitis.
Understanding the Symptoms and Signs of Diverticulitis
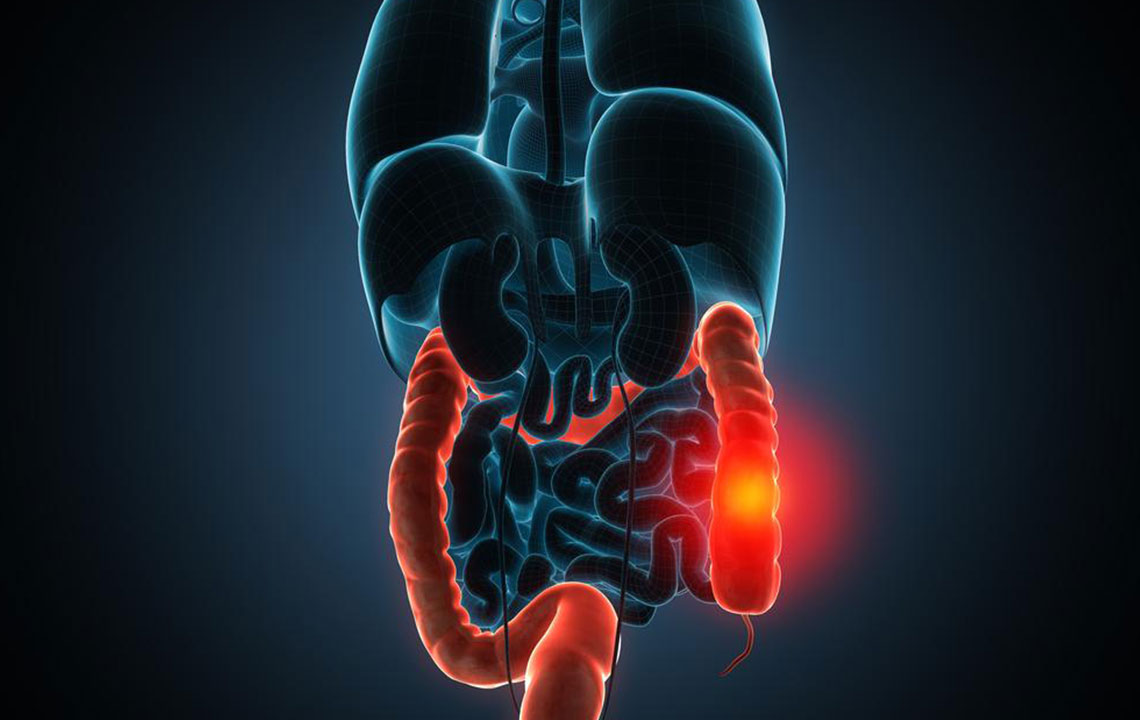
Diverticulitis is a medical condition characterized by inflammation or infection of small pouches known as diverticula that form along the lining of the large intestine, commonly referred to as the colon. These pouches, called diverticula, develop initially as part of a condition called diverticulosis, which is often asymptomatic. However, when these diverticula become inflamed or infected, the condition progresses to diverticulitis, requiring prompt medical attention.
Causes and Contributing Factors
Diverticulosis predominantly affects older adults, with the risk increasing with age. Although the precise cause of diverticulosis remains unclear, research suggests that dietary habits play a significant role. A diet low in dietary fiber is widely believed to promote the formation of diverticula. Fiber adds bulk to stool, promoting regular bowel movements and reducing pressure within the colon. Without adequate fiber intake, the colon must work harder to propel stool forward, increasing intraluminal pressure and leading to the development of diverticula. Other factors such as obesity, lack of physical activity, smoking, and certain medications may also contribute to the risk of developing diverticulitis.
Common symptoms of diverticulitis include persistent lower abdominal pain, typically localized on the left side, just below the navel. The pain may be crampy, steady, or severe, and it often worsens after eating. Bowel movements can become irregular, leading to either constipation or diarrhea. Patients may also experience bloating, abdominal tenderness, nausea, and a loss of appetite. Fever exceeding 38°C (100.4°F) is common, indicating infection. Bright red or dark rectal bleeding can occur but often resolves spontaneously. If left untreated, diverticulitis can cause serious complications such as abscess formation, perforation, peritonitis, and bowel obstruction. Severe pain, persistent fever, vomiting, and signs of bleeding require immediate medical intervention. Long-term, ongoing symptoms like bleeding or frequent bowel issues should prompt a visit to healthcare providers for proper evaluation and management.
Diagnostic Procedures for Diverticulitis
Diagnosing diverticulitis involves a combination of clinical assessment and diagnostic tests. Initially, clinicians review the patient’s history and perform a physical examination, including a digital rectal exam to check for tenderness or blood. Blood tests are conducted to detect elevated white blood cell counts, which are indicative of infections or inflammation. Imaging techniques are essential for confirming diverticulitis. A computed tomography (CT) scan of the abdomen and pelvis is considered the gold standard, as it can clearly visualize inflamed diverticula, complications like abscesses, and other abnormalities. In some cases, endoscopic procedures such as colonoscopy or sigmoidoscopy may be performed after the acute phase has subsided to rule out other conditions and assess the colon’s overall health. These procedures provide direct visualization of the intestinal interior and help confirm the diagnosis.
Effective Management and Treatment of Diverticulitis
The treatment approach for diverticulitis depends on the severity of the symptoms. Mild cases often respond well to conservative management at home. Rest, hydration, and a carefully structured diet—starting with clear liquids and gradually reintroducing solid foods—are key components of recovery. Antibiotics are frequently prescribed to treat bacterial infection, and pain management may involve over-the-counter or prescription analgesics. In cases where symptoms are severe, or complications such as perforation or abscess formation occur, hospitalization and more invasive interventions like drainage or surgery might be necessary. Lifestyle modifications are crucial in preventing recurrence, including increasing dietary fiber intake, maintaining hydration, engaging in regular physical activity, and avoiding smoking and excessive alcohol consumption. Long-term management focuses on preventing future episodes through dietary and lifestyle adjustments, regular medical follow-up, and monitoring for potential complications. Remember, timely diagnosis and appropriate treatment are essential in reducing risks and improving quality of life for diverticulitis patients.





