Comprehensive Guide to Colitis: Symptoms, Causes, and Management Strategies
This comprehensive guide explores colitis, detailing its symptoms, causes, and various treatment options. It emphasizes the importance of accurate diagnosis, tailored treatment strategies, and lifestyle modifications to manage and prevent symptoms effectively, offering valuable insights for patients and caregivers alike.

Comprehensive Guide to Colitis: Symptoms, Causes, and Management Strategies
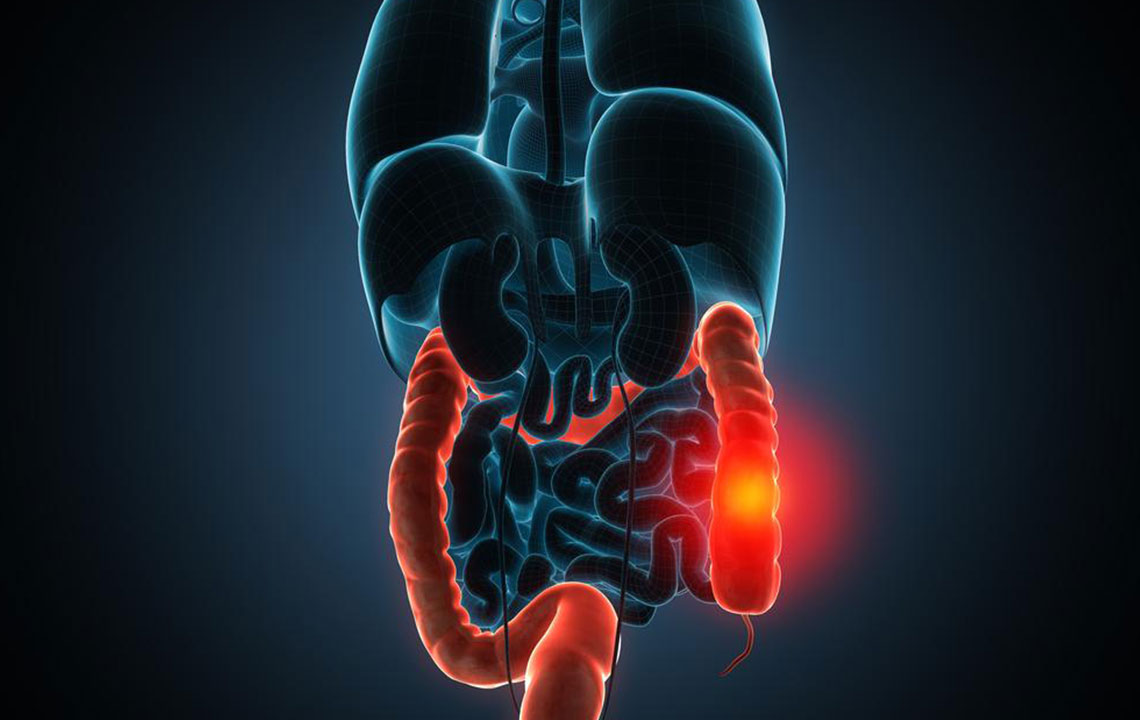
Colitis is a medical condition characterized by inflammation of the colon, which is also known as the large intestine. This condition encompasses various types, each with distinct causes, symptoms, and treatment options. Understanding these differences is crucial for effective management and relief. The primary forms include microscopic colitis, ischemic colitis, inflammatory bowel diseases such as ulcerative colitis and Crohn’s disease, chemical colitis, pseudomembranous colitis, and infectious causes—including food poisoning, bacterial infections, and parasitic infestations.
Given the diversity of colitis types, accurate diagnosis by healthcare professionals is essential. Proper identification of the form of colitis allows for targeted treatment, minimizing the risk of complications and improving patient outcomes. Symptoms often overlap, making diagnostic tests like colonoscopy, biopsies, and blood tests vital tools in determining the exact nature of the inflammation.
Recognizing the Symptoms of Colitis
The hallmark symptoms of colitis typically include diarrhea and abdominal discomfort. These signs are often the first indicators prompting individuals to seek medical attention.
Mechanisms Behind Inflammation-Induced Pain
When the colon becomes inflamed, it can lead to muscle spasms. These spasms cause episodic cramping or colicky pain, often experienced in the lower abdomen but potentially felt anywhere along the length of the colon. Inflammation disrupts the colon's ability to reabsorb water effectively, resulting in frequent, watery bowel movements, which can be distressing and disruptive. In cases such as ulcerative colitis, ulcers can form in the colon lining, leading to bleeding. This bleeding might be visible in stool or cause additional health concerns.
Pain and Urgency Associated with Diarrhea
Discomfort tends to worsen just before a bowel movement, sometimes alleviating afterward but recurring with each subsequent episode. A sudden, urgent need to defecate—known as urgency—is common, and individuals often feel a compelling urge that they cannot ignore.
Other accompanying symptoms can include:
Chills
Fever
Fatigue
Malaise
Dehydration
Dehydration symptoms might manifest as dizziness, decreased urine production, dry skin, and general weakness. Moreover, specific forms of colitis, such as Crohn’s disease and ulcerative colitis, can also produce extraintestinal manifestations, including eye inflammation, joint swelling, skin ulcers, and mouth sores. Recognizing these signs early and consulting a healthcare professional is vital for proper management.
Effective Approaches to Colitis Treatment
The treatment strategy depends heavily on the underlying cause and severity of the disease. Mild cases often respond well to symptomatic treatment, involving medications to reduce inflammation, pain relievers, and fluids to prevent dehydration, allowing the bowel to rest and recover. More severe cases may necessitate intravenous (IV) fluids, antibiotics, or surgical intervention to remove damaged tissue or correct complications.
Specific treatments include:
Ischemic Colitis: Initially managed with supportive care, primarily IV hydration. Surgery may become necessary if tissues die due to insufficient blood supply, leading to necrosis.
Infections: Viral colitis typically resolves with supportive care and hydration, whereas bacterial infections like Clostridium difficile require targeted antibiotics and anti-inflammatory medications.
Diarrhea and Abdominal Pain: A liquid diet may be recommended along with medications to control symptoms. Consulting a healthcare provider before taking any medication is essential.
Inflammatory Bowel Disease (IBD): Usually managed with anti-inflammatory drugs initially. If these are ineffective, immune suppressants or surgery might be necessary to control the disease and prevent complications.
The Role of Diet in Managing Colitis
Nutrition plays a pivotal role in managing colitis symptoms and preventing flare-ups. Eating a balanced, nutrient-rich diet can help reduce inflammation and minimize symptoms. It is advisable to avoid certain foods during flare-ups, including fried, greasy foods, high-fiber items such as nuts and seeds, and dairy products if lactose intolerance is present. Lactose-free dairy options can sometimes be tolerated better and are recommended for those with lactose sensitivity.
Preventive measures are equally important in managing colitis. Regularly monitoring blood pressure, blood sugar levels, and cholesterol, coupled with lifestyle changes such as quitting smoking, can significantly reduce the risk of disease progression and complications. For individuals diagnosed with colitis or at risk, adopting a healthy lifestyle and maintaining regular medical check-ups are crucial components of long-term management.