Comprehensive Guide to Bleeding and Clotting Disorders: Symptoms, Causes, and Management Strategies
This comprehensive guide explores bleeding and clotting disorders, covering their symptoms, causes, diagnosis, and treatment options. It emphasizes early detection, modern management strategies, natural remedies, and prevention tips for maintaining healthy blood function and preventing serious complications resulting from abnormal clotting or bleeding issues.
Comprehensive Guide to Bleeding and Clotting Disorders: Symptoms, Causes, and Management Strategies
Understanding the complexities of blood health is essential for recognizing and managing bleeding and clotting disorders. These conditions disrupt the delicate balance of our circulatory system, leading to potentially life-threatening complications if left untreated. This extensive guide will explore the fundamental aspects of bleeding and clotting disorders, including their symptoms, diverse causes, diagnostic procedures, and up-to-date treatment options. Additionally, we will discuss natural remedies that may complement conventional medical care and provide tips for prevention and early detection.
What are bleeding and clotting disorders?
Blood disorders related to bleeding and clotting encompass a wide spectrum of health issues that involve either excessive bleeding tendencies or abnormal clot formation. The body's ability to form blood clots is vital for stopping bleeding after injury. Conversely, when clotting occurs too easily or excessively, it can obstruct blood flow and damage vital organs.
Primarily, these disorders are classified into two categories: bleeding disorders, which cause abnormal bleeding, and clotting disorders, which promote unwanted clot formation. The clinical implications of these conditions are substantial, affecting cardiovascular health, tissue oxygenation, and overall wellbeing. Recognizing early symptoms and understanding the underlying causes are crucial steps toward effective management and improved prognosis.
Types of Bleeding and Clotting Disorders
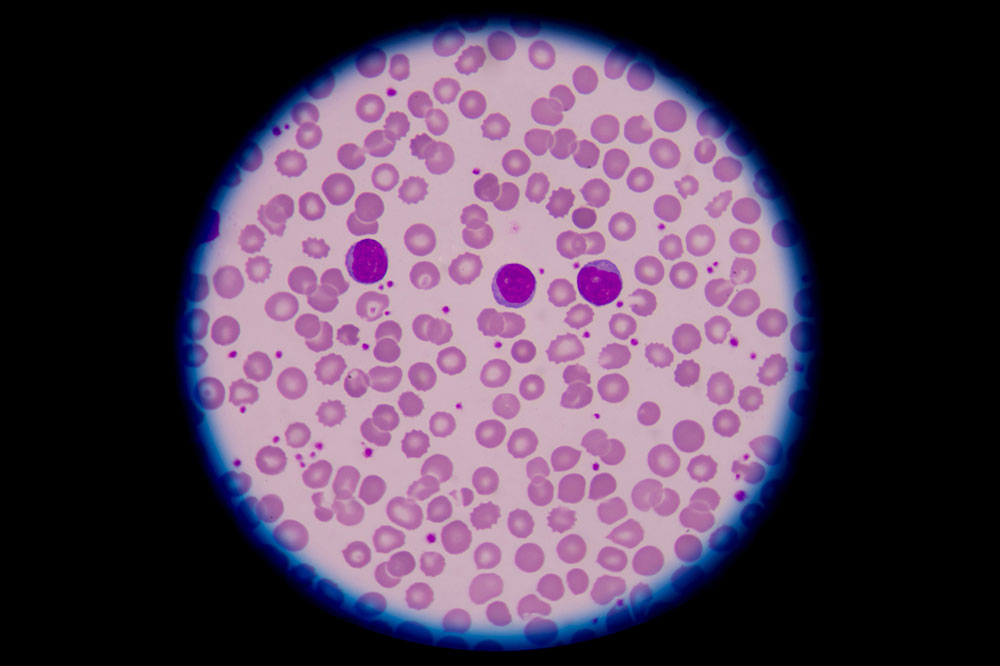
The body’s coagulation system is complex, involving numerous proteins, cells, and pathways. When any part of this system malfunctions, various disorders may arise. These are broadly categorized into:
Bleeding Disorders: These include hemophilia, von Willebrand disease, and platelet disorders. They are characterized by insufficient clot formation, leading to prolonged or spontaneous bleeding episodes.
Clotting Disorders (Thrombotic or Hypercoagulable Conditions): Also called thrombophilia, these conditions cause excessive clot formation, which increases the risk of thrombi that can obstruct blood flow. Key examples include factor V Leiden mutation, prothrombin gene mutation, antiphospholipid syndrome, and deficiencies of natural anticoagulants such as protein C, protein S, or antithrombin III.
Health Risks Associated with Clotting and Bleeding Disorders
Clotting and bleeding disorders can lead to severe health complications if unidentified or unmanaged. When a clot forms inappropriately, it can cause deep vein thrombosis (DVT), pulmonary embolism (PE), heart attacks, or strokes. Conversely, bleeding disorders may result in spontaneous hemorrhages, anemia, or increased bleeding after surgery or injury. These risks highlight the importance of early diagnosis and proper treatment to prevent long-term health issues.
Recognizing Symptoms and Risks
Symptoms vary widely depending on the specific disorder and its severity. Some individuals may remain asymptomatic, while others experience notable signs such as:
Unexplained bruising or bleeding from cuts
Prolonged bleeding after injury, dental procedures, or surgeries
Frequent nosebleeds or gum bleeding
Swelling, pain, or redness in the affected area (e.g., legs or arms)
Chest pain, shortness of breath, or rapid heartbeat indicating pulmonary embolism or heart attack
Swelling and tenderness in legs suggesting deep vein thrombosis
Causes of Bleeding and Clotting Disorders
The origins of these disorders can be broadly divided into inherited genetic factors and acquired causes. Understanding these causes helps in targeted diagnosis and customized treatment plans.
Genetic Causes: Mutations such as Factor V Leiden, Prothrombin G20210A mutation, hemophilia A and B, von Willebrand disease, and deficiencies in natural anticoagulants are inherited in families. These genetic alterations compromise the normal clotting process, either increasing or decreasing clotting tendencies.
Acquired Causes: External factors and health conditions can induce or exacerbate bleeding or clotting issues. These include surgical procedures, traumatic injuries, pregnancy, hormonal therapies, prolonged bed rest, cardiac diseases, infections, cancers, or certain medications like anticoagulants and antiplatelet drugs.
Diagnostic Procedures and Tests
Accurate diagnosis hinges on a combination of thorough medical history assessment and targeted laboratory testing. Key tests include:
Prothrombin Time (PT): Measures how quickly blood clots, helping detect clotting factor deficiencies.
Activated Partial Thromboplastin Time (aPTT): Assesses the intrinsic clotting pathway.
D-dimer Test: Detects clot presence and breakdown, useful for identifying thrombosis.
Genetic Testing: Identifies specific mutations like Factor V Leiden or prothrombin gene mutation.
Platelet Count: Checks for low platelet levels that can cause bleeding issues.
Modern Treatment Options and Management
Managing bleeding and clotting disorders requires a comprehensive approach involving medication, lifestyle adjustments, and sometimes genetic counseling. Common treatment strategies include:
Anticoagulants and Blood Thinners: Medications like warfarin, heparin, direct oral anticoagulants (DOACs) help prevent abnormal clot formation. Careful monitoring is essential to balance bleeding risk.
Replacement Therapies: Infusions of clotting factors or plasma-derived products are used in conditions like hemophilia.
Desmopressin: Used in mild hemophilia or von Willebrand disease to increase clotting factors temporarily.
Thrombectomy and Surgical Interventions: In severe cases, removal of clots may be necessary to restore blood flow.
Lifestyle Modifications: Maintaining a healthy weight, staying active, avoiding smoking, and managing comorbid conditions reduce overall risk.
Natural Remedies and Supplements
Complementary natural solutions might support blood health when used alongside conventional therapy, but should always be discussed with your healthcare provider. Some traditional remedies include:
Turmeric: Contains curcumin, which has anti-inflammatory and blood-thinning properties.
Garlic: Rich in sulfur compounds that promote blood circulation and may inhibit clot formation.
Cayenne Pepper: Contains salicylates, which naturally thin the blood.
It is important to exercise caution with natural remedies, as they can interact with medications or worsen bleeding tendencies. Always consult your healthcare provider before starting any supplement or herbal treatment.
Preventing Bleeding and Clotting Disorders
Prevention focuses on early detection, lifestyle choices, and managing risk factors. Regular health screenings, especially if there's a family history of blood disorders, are vital. Maintaining a balanced diet rich in vitamins K and C, staying hydrated, avoiding pro-thrombotic and bleeding-inducing substances, and adhering to medical advice significantly reduce risks.