Ultimate Guide to Blood Disorders: Symptoms, Causes, Diagnosis, and Treatment
This comprehensive guide details blood disorders, including symptoms, causes, types, and treatment options. Learn how early diagnosis and personalized management can improve health outcomes for conditions like anemia, leukemia, and clotting disorders. Stay informed on the latest therapies and preventative strategies for optimal blood health.
Comprehensive Overview of Blood Conditions and Their Management
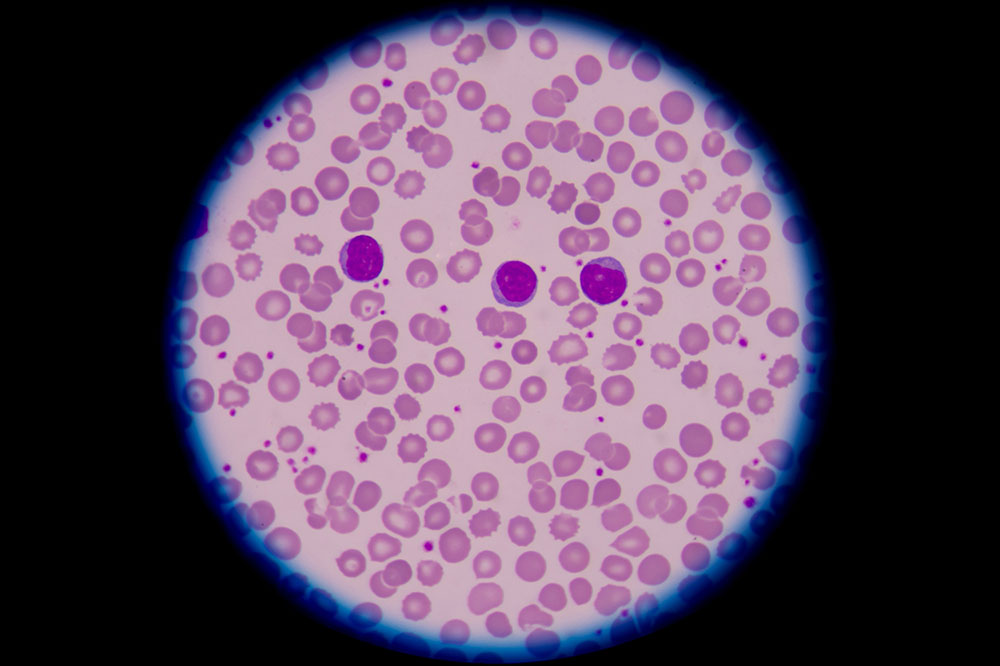
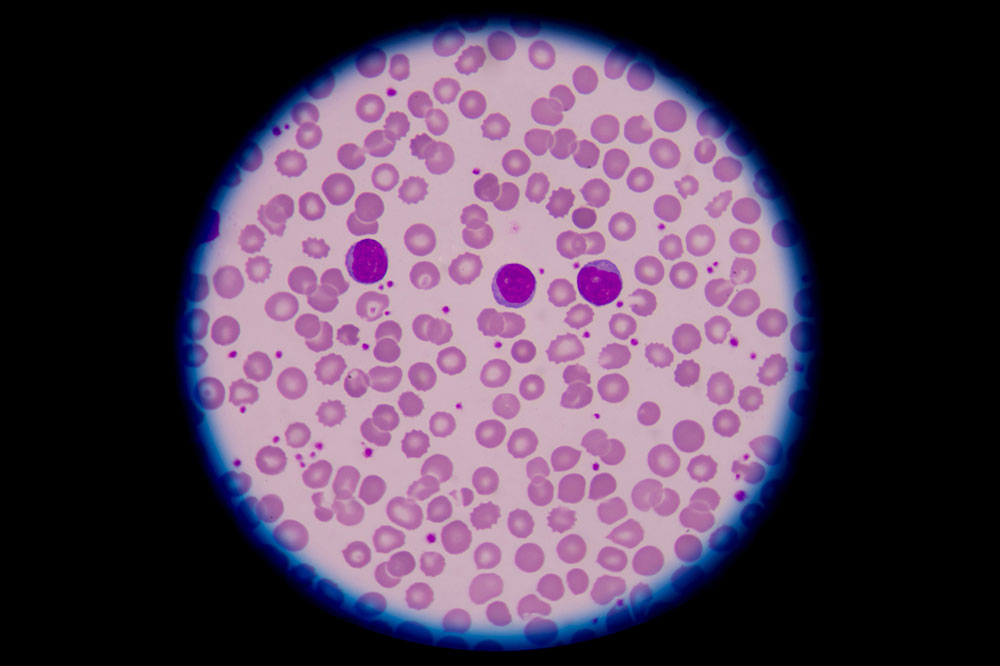
Blood health is fundamental to overall wellness, and any disruption in blood components or bone marrow function can lead to a spectrum of health issues. Blood disorders encompass a wide range of medical conditions that affect the cellular components of blood—including red blood cells, white blood cells, and platelets—as well as plasma clotting factors. The bone marrow, residing within the bones, is responsible for producing these vital cells. When anomalies occur in their production, function, or lifespan, it can result in conditions that impair immune defenses, oxygen transport, and the blood’s ability to clot properly.
Understanding the intricacies of blood disorders—their symptoms, causes, classification, and available treatment options—is crucial for early diagnosis and effective management. This comprehensive guide aims to provide in-depth information to inform patients, caregivers, and healthcare professionals about these complex conditions, highlighting recent advances and approaches for optimal care.
Recognizing the Signs and Symptoms of Blood Disorders
The symptomatology of blood disorders varies significantly depending on which component of the blood is affected. Since each blood element performs vital functions, its impairment manifests in distinctive ways. Recognizing these symptoms early can prompt timely medical intervention, preventing complications and improving prognosis.
Generally, symptoms can be categorized into the effects of red blood cell deficiencies, white blood cell dysfunctions, or platelet abnormalities:
Anemia and Red Blood Cell Disorders: Patients often experience persistent fatigue, weakness, shortness of breath, dizziness, pallor, cold extremities, and a rapid or irregular heartbeat. These symptoms stem from insufficient oxygen delivery to tissues caused by decreased red blood cell count or hemoglobin levels.
White Blood Cell Abnormalities: Conditions affecting white blood cells can compromise immunity, leading to recurrent or severe infections, fever, weight loss, night sweats, and delayed wound healing. Leukemia and lymphoma are examples characterized by abnormal proliferation or destruction of white blood cells.
Platelet or Clotting Disorders: These lead to bleeding tendencies such as easy bruising, frequent nosebleeds, bleeding gums, prolonged bleeding from minor cuts, and the formation of petechiae. In some cases, wounds may resist healing or reopen, indicating clotting dysfunctions.
Classification and Underlying Causes of Blood Disorders
Blood disorders are typically classified based on which component of the blood is affected. While some disorders are inherited, acquired conditions caused by environmental or lifestyle factors are also prevalent. Recognizing the root causes is vital for diagnosis and treatment planning.
Most blood disorders originate from genetic predispositions but can also develop due to environmental influences, infections, toxins, medications, nutritional deficiencies, or bone marrow problems. Common categories include:
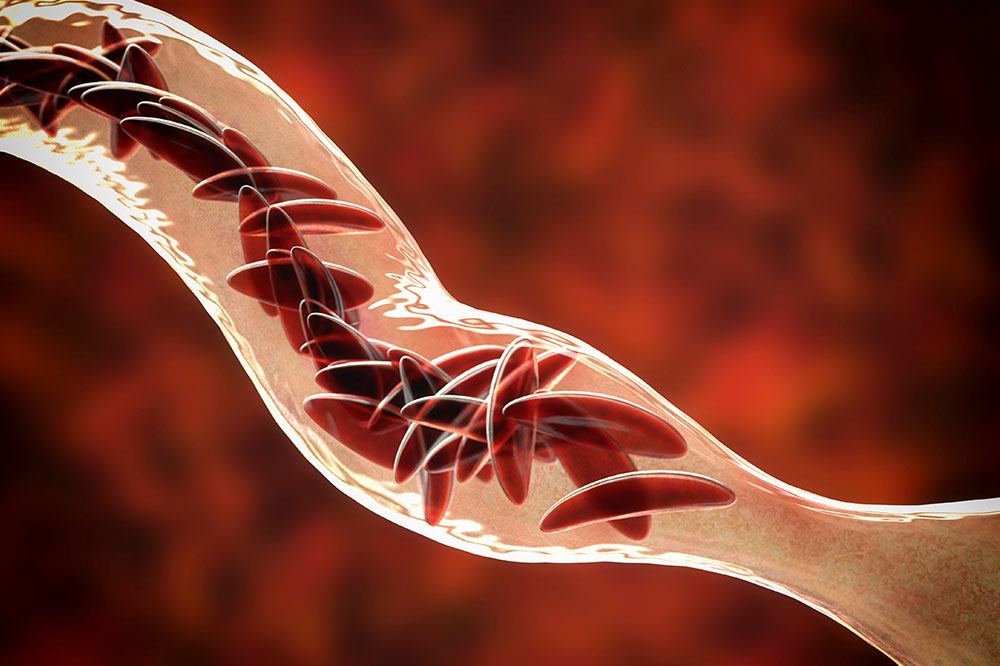
Red Blood Cell Disorders: These interfere with oxygen transportation throughout the body. Anemia, characterized by low red blood cell count or hemoglobin deficiency, is the most common. Other conditions include thalassemia, a hereditary blood disorder causing abnormal hemoglobin synthesis, and polycythemia vera, where excess red blood cells increase blood viscosity and risk of clots.
White Blood Cell Disorders: These affect immune system function and include leukemias, lymphomas, and myelodysplastic syndromes. Leukemia involves uncontrolled proliferation of abnormal white blood cells, compromising immunity and increasing infection risk. Lymphomas are cancers originating in lymph nodes, and myelodysplastic syndromes involve ineffective blood cell production.
Platelet and Coagulation Disorders: Abnormal platelet counts or dysfunctions lead to bleeding or clotting issues. Hemophilia and von Willebrand disease are inherited conditions that impair clot formation. Thrombocytopenia, a low platelet count, can occur due to autoimmune diseases, infections, or certain medications, resulting in bleeding risks.
Plasma Cell Disorders: These involve abnormal plasma cells, which produce excessive or defective antibodies. Multiple myeloma, a common plasma cell malignancy, can cause bone pain, anemia, kidney dysfunction, and increased infection susceptibility.
Effective Treatment Strategies for Blood Disorders
Treatment options are tailored to each specific blood disorder, taking into account the severity, patient's age, overall health, and underlying causes. The goal is to correct blood cell deficiencies, control symptoms, and prevent complications.
Some conditions may require no immediate intervention but necessitate ongoing management; others demand aggressive therapy.
Key therapeutic approaches include:
Vitamin and Mineral Supplements: Iron supplements for iron-deficiency anemia, vitamin B12 injections, or folic acid therapy are used to replenish deficiencies contributing to anemia.
Blood Transfusions: To rapidly increase red blood cell or platelet counts in severe cases, transfusions are often necessary.
Medications: Erythropoietin-stimulating agents promote red blood cell production; corticosteroids may be used in certain autoimmune disorders; chemotherapy and targeted therapies are options for blood cancers.
Clotting Factor Replacement: Hemophilia patients benefit from infusions of clotting factors; plasma exchanges may be used in certain conditions.
Bone Marrow Transplantation: For some blood cancers and marrow failure syndromes, stem cell transplants can be curative.
Supportive Care and Lifestyle Adjustments: Managing infections, avoiding trauma, and maintaining a nutritious diet aid overall health and achieve better outcomes.
Emerging therapies like gene therapy and targeted immunotherapies are offering new hope for patients with previously intractable blood disorders. It is crucial for patients to work closely with hematologists to determine the most appropriate treatment plan based on their unique situation.
Early diagnosis and personalized treatment can significantly improve quality of life, reduce complications, and potentially achieve remission or cure in some cases. Staying informed about advances in blood disorder management remains essential for patients and healthcare providers alike.