Comprehensive Strategies for Managing Type 2 Diabetes in Adults
This comprehensive guide discusses effective strategies for managing type 2 diabetes in adults, emphasizing lifestyle changes, medication options, diet tips, and preventive measures. It aims to help individuals understand their condition and adopt a proactive approach to control blood sugar levels, reduce complications, and maintain quality of life through evidence-based practices and personalized care.

Effective Approaches to Understanding and Managing Type 2 Diabetes in Adults
Type 2 diabetes mellitus (T2DM) is a widespread metabolic disorder that continues to pose significant health challenges worldwide. Previously referred to as adult-onset diabetes or non-insulin-dependent diabetes, it primarily affects the body's ability to regulate blood glucose levels effectively. The condition develops when the body either becomes resistant to insulin's effects or does not produce enough insulin to meet its needs, leading to elevated blood sugar levels that can damage organs and tissues over time.
Understanding the scope of type 2 diabetes is crucial, especially considering its alarming prevalence. Currently, approximately 29.1 million people in the United States are living with diabetes, and out of this population, about 8.1 million remain undiagnosed. The annual increase in new cases is roughly 1.4 million, underscoring the pressing need for better awareness, early detection, and effective management strategies.
One of the defining challenges of T2DM is its often insidious onset. Symptoms tend to develop gradually, making early diagnosis difficult but vital to prevent long-term complications. Typical signs and symptoms include frequent urination, persistent thirst, unexplained weight loss, chronic fatigue, blurred vision, increased susceptibility to infections, slow-healing cuts or sores, and skin discoloration known as acanthosis nigricans. Recognizing these symptoms early can significantly improve health outcomes through timely intervention.
Managing type 2 diabetes involves a multifaceted approach centered around lifestyle modifications, dietary regulation, and, when necessary, pharmacotherapy. The goal is to maintain blood glucose levels within a target range to prevent complications such as cardiovascular disease, nerve damage, kidney failure, and vision impairment.
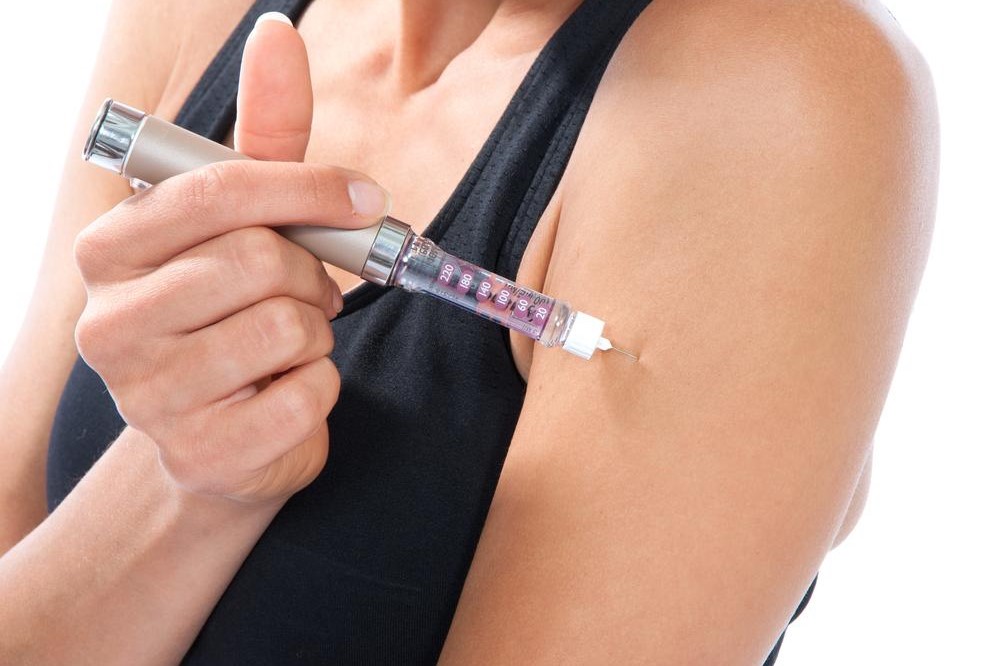
Medication options are diverse and tailored to individual patient needs. Common drug classes include Sulfonylureas, which stimulate insulin release; Meglitinides, which also enhance insulin secretion; Thiazolidinediones, which improve insulin sensitivity; DPP-4 inhibitors; GLP-1 receptor agonists; SGLT2 inhibitors; and insulin therapy in advanced cases. The choice of medication depends on factors like blood sugar levels, presence of comorbidities, and patient lifestyle.
Alongside medication, diet plays a fundamental role in managing T2DM. Adopting a consistent meal schedule helps stabilize blood glucose fluctuations. Emphasizing nutrient-dense foods such as high-fiber carbohydrates—including whole grains, legumes, and vegetables—facilitates slower glucose absorption. Incorporating omega-3 fatty acids and healthy fats from sources like fish, nuts, and seeds supports overall health.
Conversely, certain foods should be limited or avoided entirely. These include saturated fats, trans fats, processed meats, sugary beverages, high-fat dairy products, fried foods, and salty snacks. Reducing intake of processed and fast foods helps control calorie consumption and prevents spikes in blood sugar levels.
Complementing dietary changes, engaging in regular physical activity is essential for effective blood sugar management. Exercise helps increase insulin sensitivity, promote weight loss, and improve cardiovascular health. Recommended activities include brisk walking, cycling, swimming, or aerobic exercises performed at least 150 minutes per week. Consult a healthcare provider before initiating new exercise routines, especially for individuals with existing health issues.
Stress management and adequate sleep are additional elements that influence blood sugar control. Techniques such as mindfulness, meditation, and relaxation exercises can reduce stress hormones that elevate blood glucose. Ensuring quality sleep supports metabolic health and enhances overall well-being.
While lifestyle modifications can significantly impact sugar regulation, some patients may require medical interventions when lifestyle changes alone are insufficient. Regular blood sugar monitoring helps track progress and adjust treatment plans. Healthcare providers may recommend personalized medication regimens, insulin therapy, or a combination of approaches to achieve optimal control.
Preventive measures extend beyond individual treatment. Routine health screenings, including blood glucose tests and HbA1c assessments, are vital for early detection and ongoing management. Maintaining a healthy weight, avoiding tobacco use, limiting alcohol consumption, and managing other health conditions like hypertension and dyslipidemia are important components of comprehensive diabetes care.
In conclusion, managing type 2 diabetes in adults requires a proactive and educated approach. Combining dietary discipline, physical activity, regular monitoring, and appropriate medication adherence enables individuals to lead active, healthy lives despite their diagnosis. With advances in medical knowledge and technology, personalized treatment plans can significantly improve quality of life and reduce the risk of severe complications. Empowering patients through education and support systems is fundamental to achieving successful diabetes management in the modern era.