Comprehensive Guide to Managing Diabetes and Achieving a Healthy Lifestyle
Learn comprehensive strategies for managing diabetes effectively, including understanding the different types, recognizing symptoms, exploring treatment options, and adopting lifestyle modifications. This guide provides essential insights to improve quality of life and prevent complications associated with diabetes, emphasizing personalized care and ongoing health monitoring for optimal management.

Strategies for Effective Diabetes Management and Overall Well-being
Diabetes mellitus is a chronic and complex metabolic disorder characterized by the body's inability to regulate blood glucose levels effectively. This condition arises when the pancreas fails to produce sufficient insulin or when the body's cells become resistant to insulin's effects, disrupting the normal process of glucose utilization. Proper management of diabetes is critical, not only to control blood sugar levels but also to prevent long-term complications affecting various organ systems. These complications include damage to the eyes (diabetic retinopathy), kidneys (diabetic nephropathy), nerves (diabetic neuropathy), and increased risks of cardiovascular diseases such as heart attacks and strokes. This comprehensive guide aims to detail the types of diabetes, their symptoms, causes, risk factors, treatment options, and lifestyle strategies to promote optimal health for individuals living with diabetes.
Understanding Different Types of Diabetes
Type 1 Diabetes:
Type 1 diabetes is an autoimmune condition where the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. This leads to a deficiency of insulin, which is vital for transporting glucose from the bloodstream into cells for energy. The exact cause of this autoimmune response remains unclear, but it is believed to involve genetic predisposition combined with environmental triggers, such as viral infections. Individuals with type 1 diabetes require lifelong insulin therapy—either through injections or continuous pump delivery—to maintain normal blood sugar levels. It is typically diagnosed in children and young adults, making it a lifelong condition that necessitates daily management.
Type 2 Diabetes: This is the most common form of diabetes, accounting for about 90-95% of all cases. Unlike type 1, the pancreas still produces insulin; however, the body's cells become resistant to insulin’s effects, leading to impaired glucose uptake. This results in elevated blood sugar levels. The rise in type 2 cases correlates strongly with lifestyle factors such as obesity, physical inactivity, poor diet, and aging. Managing type 2 diabetes often involves a combination of lifestyle changes, oral medications, and sometimes insulin therapy to control blood glucose effectively.
Prediabetes: Prediabetes is a condition where blood glucose levels are higher than normal but do not yet meet the diagnostic criteria for diabetes. Fasting blood sugar levels range from 100 to 125 mg/dL, and the oral glucose tolerance test shows elevated results. Prediabetes is a warning sign that diabetes may develop if lifestyle interventions are not implemented. It provides an important window for preventative action, emphasizing weight loss, diet, and increased physical activity to reverse or halt progression.
Normal fasting blood sugar levels are between 70-99 mg/dL. Levels exceeding 126 mg/dL after fasting typically indicate diabetes. Blood sugar readings between 100-125 mg/dL denote prediabetes, serving as a precursor to full-blown diabetes.
Gestational Diabetes: This condition occurs during pregnancy when hormonal changes induce insulin resistance. It affects pregnant women and can increase the risk of complications during labor and delivery. While gestational diabetes often resolves postpartum, women who experience it are at higher risk of developing type 2 diabetes later in life. Regular blood sugar monitoring during pregnancy and postpartum follow-up are essential to prevent adverse outcomes.
Understanding the specific types of diabetes helps in tailoring management strategies effectively. Consulting healthcare professionals for diagnosis and personalized treatment plans is crucial for optimal health outcomes.
Recognizing Common Symptoms of Diabetes
Symptoms can vary depending on the type and severity of the condition but generally include increased thirst (polydipsia), persistent hunger (polyphagia), unexplained weight loss, fatigue, blurred vision, and frequent urination (polyuria). Individuals may also experience slow-healing sores, frequent infections, and dry skin. Men might suffer from reduced libido, erectile dysfunction, or urinary tract infections, whereas women may experience recurrent yeast infections, urinary tract infections, or vaginal dryness.
Specific symptoms associated with different types include:
Type 1: Intense thirst and hunger, rapid weight loss despite increased appetite, fatigue, blurred vision, frequent urination, mood swings, and irritability.
Type 2: Similar symptoms but often accompanied by recurring infections, slow wound healing, tingling or numbness in extremities, and symptoms exacerbated by obesity or sedentary lifestyle.
Gestational Diabetes: Often asymptomatic but may present with increased thirst, fatigue, or urinary frequency. Diagnosis is usually made through glucose testing during pregnancy.
Understanding causes and risk factors for diabetes is vital. Factors include genetic predisposition, unhealthy diet, physical inactivity, obesity, age over 45, high blood pressure, high cholesterol levels, and family history. Women with a history of gestational diabetes or previous large babies are at increased risk.
Effective management of diabetes involves a combination of medication, lifestyle adjustments, and monitoring. Treatment goals focus on maintaining blood glucose levels within target ranges to prevent complications.
Medical Treatment Options for Diabetes
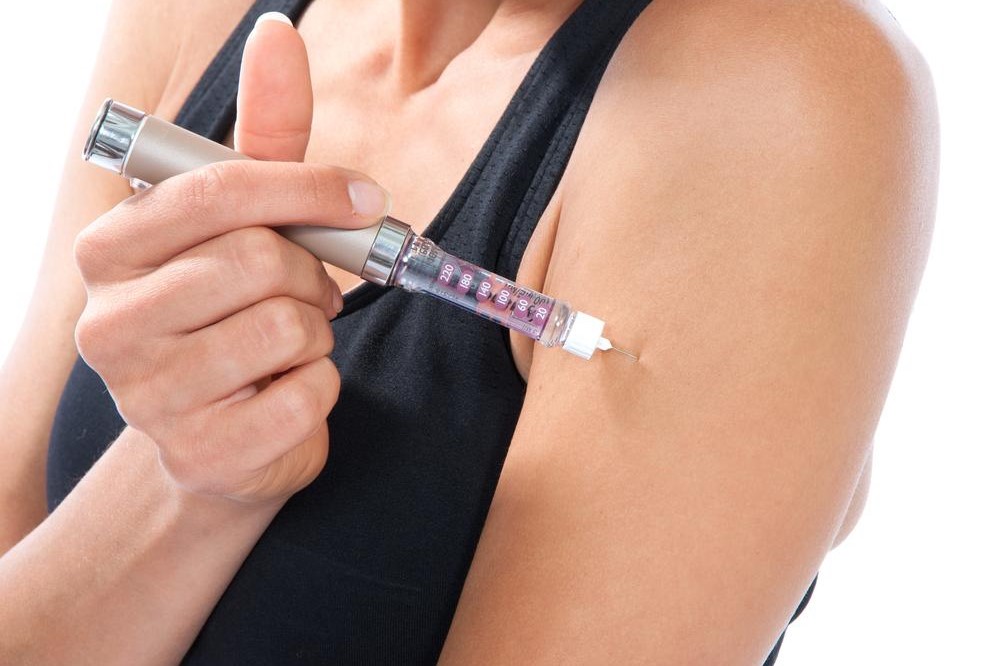
Insulin therapy remains a cornerstone for managing type 1 diabetes and is often necessary for type 2 diabetes individuals with advanced disease. Different types of insulin—long-acting, rapid-acting, and premixed formulations—are administered via daily injections or insulin pumps. New technologies like tubeless insulin pumps and smart insulin pens have improved convenience and precision. Insulin cannot be taken orally because of its degradation in the gastrointestinal tract, necessitating injection methods.
In type 2 diabetes, oral medications are first-line treatments and include drugs that stimulate insulin release (sulfonylureas, meglitinides), improve insulin sensitivity (metformin, thiazolidinediones), or reduce glucose production in the liver. Recently, injectable agents like GLP-1 receptor agonists have gained popularity due to their additional benefits in weight management and cardiovascular risk reduction.
In some cases, further interventions such as bariatric surgery or pancreas transplantation are considered, particularly for obese patients with uncontrolled diabetes or those who experience severe complications.
Lifestyle Changes and Natural Remedies to Support Diabetes Management
Adopting a healthy lifestyle is fundamental in managing and potentially reversing type 2 diabetes. A balanced diet emphasizes whole grains, lean proteins, healthy fats, and plenty of vegetables and fruits. Reducing intake of sugars, processed foods, and fried items helps prevent blood sugar spikes. Limiting alcohol consumption is also advisable.
Regular physical activity—targeting at least 150 minutes of moderate exercise weekly—improves insulin sensitivity, aids weight loss, and boosts overall well-being. Activities like brisk walking, cycling, swimming, or yoga can be effective.
Weight management is crucial; even modest weight loss of 5-10% can significantly improve blood sugar control and may lead to remission in some cases. Natural remedies such as fatty fish rich in omega-3 fatty acids (like salmon), leafy greens, eggs, chia seeds, turmeric, Greek yogurt, and nuts have anti-inflammatory properties and support metabolic health.
Managing stress through mindfulness, meditation, and adequate sleep also positively impacts blood sugar levels. Avoiding sugary, fried, and processed foods and maintaining hydration are key lifestyle components.
Early detection through regular screening, especially for individuals at high risk, combined with these lifestyle interventions, can delay or prevent the progression of diabetes. Emphasizing education and continuous monitoring helps individuals stay vigilant and empowered to live healthier lives with diabetes.