Comprehensive Guide to Insulin Therapy: Essential Strategies for Effective Diabetes Management
This in-depth article discusses the essential aspects of insulin therapy for diabetes management, including the types of insulin, delivery methods, and personalized treatment approaches. It highlights the importance of insulin in regulating blood sugar levels, explains various insulin formulations, and offers guidance on selecting appropriate regimens for optimal health. Perfect for patients and healthcare providers alike, this comprehensive guide emphasizes the advancements in insulin treatment and its critical role in preventing diabetes-related complications. A must-read for effective disease management.

Comprehensive Guide to Insulin Therapy: Essential Strategies for Effective Diabetes Management
Managing diabetes effectively requires a thorough understanding of insulin therapy—a cornerstone treatment for both type 1 and type 2 diabetes. With advancements in medical technology and personalized treatment plans, insulin therapy has become more adaptable and effective than ever before. This comprehensive guide explores the various aspects of insulin therapy, including its types, methods of delivery, and the critical role it plays in maintaining optimal blood glucose levels. Whether you are newly diagnosed or looking to better manage your condition, understanding insulin therapy is vital for leading a healthy lifestyle.
Insulin therapy is a medical treatment involving the administration of insulin, a hormone that regulates blood sugar levels. For individuals with type 1 diabetes, the pancreas produces little to no insulin, necessitating external supplementation to sustain normal physiological functions. Meanwhile, many type 2 diabetes patients may eventually require insulin due to insulin resistance or declining pancreatic function. Personalized insulin regimens are tailored to individual needs to ensure effective blood glucose control and prevent long-term complications.
Understanding the Role of Insulin in Diabetes Management
Insulin is a crucial hormone naturally produced by the pancreas. It facilitates the entry of glucose from the bloodstream into cells, providing energy for bodily functions. In a healthy individual, insulin production is finely tuned to prevent high or low blood sugar levels. However, in diabetes, this regulation is impaired. In type 1 diabetes, the immune system attacks insulin-producing beta cells, leading to minimal or no insulin production. Conversely, in type 2 diabetes, the body's cells become less responsive to insulin—a condition known as insulin resistance—forcing the pancreas to produce more insulin initially, but eventually leading to decreased secretion.This disruption in insulin function causes abnormal blood sugar levels, which can result in a variety of health issues such as cardiovascular disease, kidney damage, nerve damage, and vision problems if poorly managed. External insulin therapy becomes necessary to restore proper glucose regulation, preventing hyperglycemia and its associated risks. The main goal of insulin therapy is to simulate natural insulin release as closely as possible to maintain blood sugar levels within a target range.
Types of Insulin and Their Unique Characteristics
Insulin comes in several formulations, each designed to mimic different aspects of natural insulin secretion. These varieties are categorized based on their onset of action, peak activity, and duration:
Rapid-acting insulin: Usually begins working within 15 minutes of injection, peaks at about 1 hour, and lasts between 3 to 5 hours. It is often used for mealtime coverage. Examples include insulin aspart, insulin glulisine, and insulin lispro.
Short-acting insulin: Starts to work within 30 to 60 minutes, peaks around 2 to 3 hours, and lasts 5 to 8 hours. Regular insulin is a typical example, suitable for controlling blood sugar around meal times.
Intermediate-acting insulin: Initiates action in 1 to 3 hours, peaks in 4 to 12 hours, and lasts 12 to 16 hours. NPH insulin falls into this category and is often used in combination with other insulins.
Long-acting insulin: Begins to work approximately one hour after injection, with a relatively flat peak, lasting between 20 to 26 hours. Examples include insulin glargine and insulin detemir, often used to provide basal insulin coverage throughout the day.
Premixed insulin: Combines rapid or short-acting insulin with intermediate-acting insulin, offering convenience for patients seeking simplified regimens.
Insulin Therapy Modalities: Personalizing Treatment Plans
Developing an effective insulin therapy plan involves choosing appropriate types and delivery methods based on individual lifestyle, health status, and preferences. Main approaches include:
Once-daily injections: Typically use long-acting or intermediate-acting insulin to provide a basal level of insulin throughout the day and night. Suitable for many patients with type 2 diabetes seeking simplicity.
Multiple daily injections (MDI): Involves injecting rapid- or short-acting insulin around meal times, along with a long-acting insulin for basal coverage. This approach offers more flexibility and tighter glucose control, often recommended for people with both type 1 and type 2 diabetes.
Insulin pump therapy: Uses a portable device that continuously delivers insulin through a catheter inserted beneath the skin. Pumps can deliver both basal and bolus doses, mimicking natural insulin secretion closely.
Choosing the right insulin regimen depends on factors such as blood sugar patterns, lifestyle, dietary habits, and existing health conditions. A healthcare professional can tailor a plan that balances efficacy with convenience and minimizes the risk of hypoglycemia.
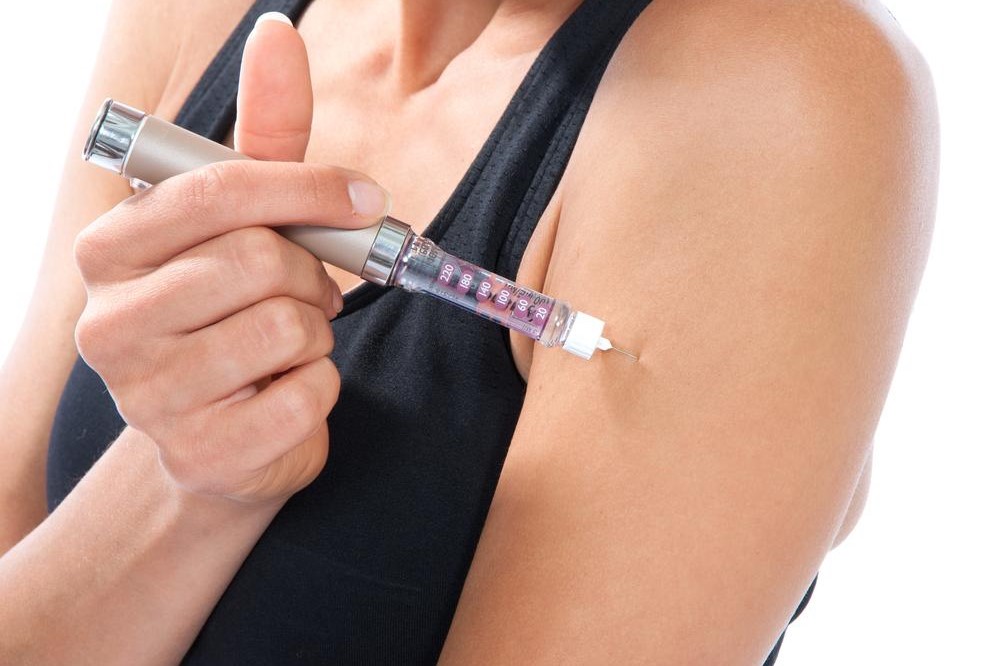
Delivery Methods: How Insulin Reaches Your Body
Insulin can be administered via various methods to suit user preferences and medical advice:
Insulin pens: Compact, user-friendly devices that allow for precise dosing with ease of use, making daily injections more comfortable.
Syringes: The traditional method, used to draw insulin from vials. Still common in some settings due to cost-effectiveness.
Insulin pumps: Continuous subcutaneous insulin infusion devices that provide rapid, adjustable insulin delivery, improving glucose management and lifestyle flexibility.
Intravenous infusion: Used in hospital settings for rapid absorption under medical supervision, primarily for acute management or during surgeries.
Insulin therapy's success depends heavily on proper administration and adherence to prescribed regimens. Healthcare providers ongoing evaluations to optimize doses and prevent complications like hypoglycemia (dangerously low blood sugar levels).In conclusion, insulin therapy remains a vital component of comprehensive diabetes care. Advances in insulin types, delivery devices, and personalized treatment plans continue to enhance quality of life for millions worldwide. Educating patients on their options and proper management strategies is essential for achieving optimal health outcomes and preventing long-term complications associated with diabetes.