Comprehensive Guide to Graves' Disease: Recognizing Symptoms and Achieving Accurate Diagnosis
This detailed guide offers a comprehensive overview of Graves' disease, covering its symptoms, diagnosis, and treatment options. It highlights the importance of early recognition and medical intervention to prevent serious complications such as eye and skin issues, and provides essential insights for patients and healthcare providers alike. With a focus on symptom recognition and diagnostic strategies, the article aims to promote awareness and improved management of this autoimmune thyroid disorder.
Comprehensive Understanding of Graves' Disease: Symptoms, Diagnosis, and Management
Graves' disease is a complex autoimmune disorder that primarily causes hyperthyroidism, a condition where the thyroid gland produces an excessive amount of thyroid hormones. This condition predominantly affects women around 40 years of age, although it can also occur in men or younger individuals. The precise cause of Graves' disease remains unknown, making it a challenging condition to predict or prevent. Since thyroid hormones regulate vital bodily functions, including metabolism, mood, temperature regulation, and nervous system activity, an imbalance can lead to serious health issues if left untreated. Early detection and effective management are critical to prevent complications such as significant weight loss, severe mood swings, depression, fatigue, and potentially life-threatening conditions.
The symptoms of Graves' disease can vary widely, ranging from the characteristic signs to less common manifestations that may be overlooked. Recognizing these symptoms early enables timely medical intervention, improving outcomes and quality of life for affected individuals. Understanding the full spectrum of symptoms—both typical and rare—is essential for patients and healthcare providers alike.
Common Symptoms of Graves' Disease include a variety of clinical features that can alert individuals and clinicians to the possibility of hyperthyroidism caused by Graves' disease. These symptoms involve multiple body systems and often present concurrently:
Excessive sweating: Patients typically experience profuse sweating, even in normal or cool environments.
Rapid or irregular heartbeat: Palpitations are common, sometimes accompanied by chest discomfort.
Unexplained weight loss: Significant weight reduction occurs despite normal or increased appetite.
Hand tremors: Fine shaking or tremors, especially noticeable in the fingertips, are typical.
Chronic fatigue: Despite restful sleep, individuals may feel overwhelmingly tired.
Anxiety and nervousness: Feelings of restlessness or irritability often occur.
Heat intolerance: Patients find it difficult to tolerate warm temperatures.
Gastrointestinal disturbances: Increased frequency of diarrhea or bowel movements is common.
Mood swings: Fluctuations in emotional states, including irritability or depression, may be observed.
Enlarged thyroid gland (goiter): The thyroid becomes visibly swollen, sometimes palpable upon examination.
Menstrual irregularities: Changes in menstrual cycle patterns, such as lighter or missed periods, are prevalent.
Sleep disturbances: Insomnia or restless sleep are often reported.
Less Common and Rare Symptoms of Graves' disease include very specific manifestations that may indicate the development of ocular or skin conditions associated with the disease:
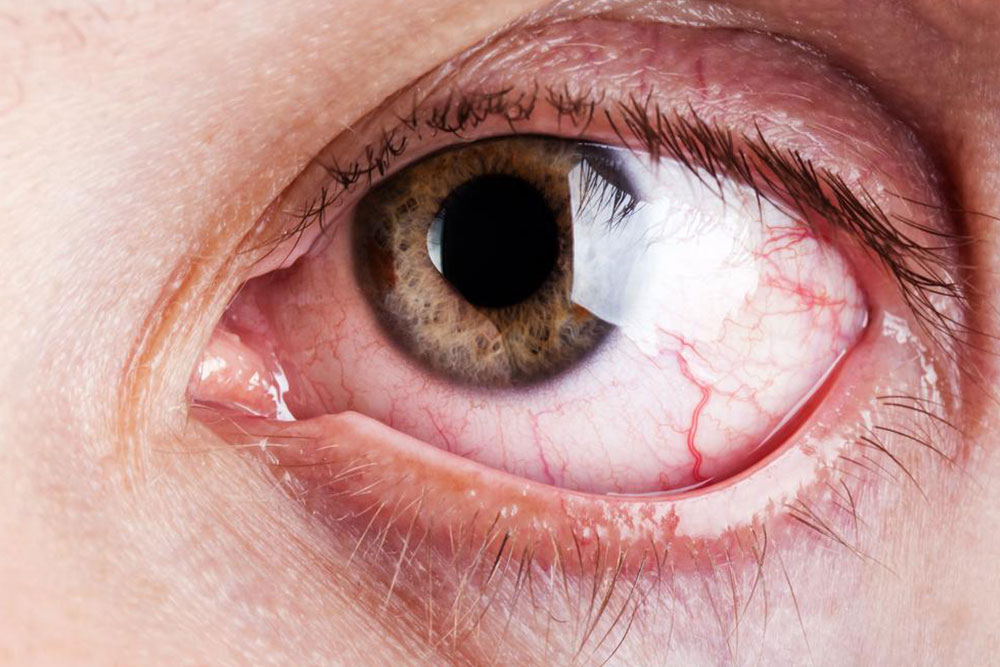
Graves' Ophthalmopathy (Eye Involvement): Affecting approximately 30% of patients, this complication involves inflammation and tissue expansion behind or around the eyes, causing:
Protruding eyes (exophthalmos): The eyeballs appear to bulge outward, which can be permanent or fluctuating.
Eye pain or pressure: Discomfort around the eyes, especially when moving or blinking.
Light sensitivity (photophobia): Increased discomfort in bright environments.
Redness and swelling: The eyelids and conjunctiva might become inflamed.
Visual disturbances: Including blurred vision, double vision, or loss of sight in severe cases.
Swollen eyelids: Edema in the eyelids can add to the discomfort or aesthetic concerns.
Graves' Dermopathy: Characterized by thickening, redness, or inflammation of the skin, particularly over the shins and the area around the feet, often resembling skin that has thickened and become rubbery. While usually mild, this skin manifestation can be cosmetically concerning but is typically manageable with topical treatments.
Understanding the severity and variability of symptoms is vital, as it influences both diagnosis and treatment. Misdiagnosis or delayed diagnosis can lead to worsening health conditions, making awareness crucial for both patients and practitioners.
Diagnosis and Treatment Strategies for Graves' Disease are multifaceted, requiring an accurate assessment of clinical features combined with laboratory and imaging tests. Consulting a healthcare provider, particularly an endocrinologist, is essential for proper diagnosis and management plan development. Diagnostic procedures include:
Blood tests: Measuring levels of thyroid hormones (free T4, free T3) and thyroid-stimulating hormone (TSH). Elevated thyroid hormones with suppressed TSH typically indicate hyperthyroidism.
Thyroid antibody tests: Detecting anti-TSH receptor antibodies confirms autoimmune activity characteristic of Graves’ disease.
Radioactive iodine uptake scan: Assesses the activity of the thyroid gland by evaluating how much iodine the gland absorbs, distinguishing Graves’ disease from other causes of hyperthyroidism.
Thyroid ultrasound: Imaging to evaluate the structure of the thyroid and detect any nodules or irregularities.
Physical examination: Evaluating the size, consistency, and tenderness of the thyroid gland, alongside assessment of eye and skin findings.
Once diagnosed, treatment options aim to normalize thyroid hormone levels and manage symptoms:
Anti-thyroid medications: Drugs like methimazole or propylthiouracil inhibit hormone production, often used as initial therapy.
Radioactive iodine therapy: Oral radioactive iodine destroys overactive thyroid tissue, leading to reduced hormone production, usually followed by hormone replacement therapy.
Surgical intervention: Thyroidectomy, the surgical removal of part or all of the thyroid gland, considered in cases where medication or radiation are unsuitable or ineffective.
Lifestyle modifications: Including dietary adjustments, stress management, avoiding triggers that worsen symptoms, and regular monitoring of thyroid function.
Managing Graves' disease requires a comprehensive approach that combines medical treatment, lifestyle changes, and ongoing monitoring to prevent complications and improve quality of life. Early diagnosis is key to achieving optimal health outcomes, reducing the risk of ophthalmic and dermatological problems, and minimizing long-term morbidity.





