Comprehensive Guide to Managing and Treating Dry Eye Syndrome Effectively
Dry eye syndrome can cause significant discomfort and impact daily life. This comprehensive guide explores the causes, symptoms, and diverse treatment options, including artificial tears, punctal plugs, LipiFlow, lifestyle changes, and nutritional support. Understanding and managing this common condition can help restore eye comfort and protect your vision. Early diagnosis and personalized care are crucial for effective relief and long-term eye health.

Comprehensive Guide to Managing and Treating Dry Eye Syndrome Effectively
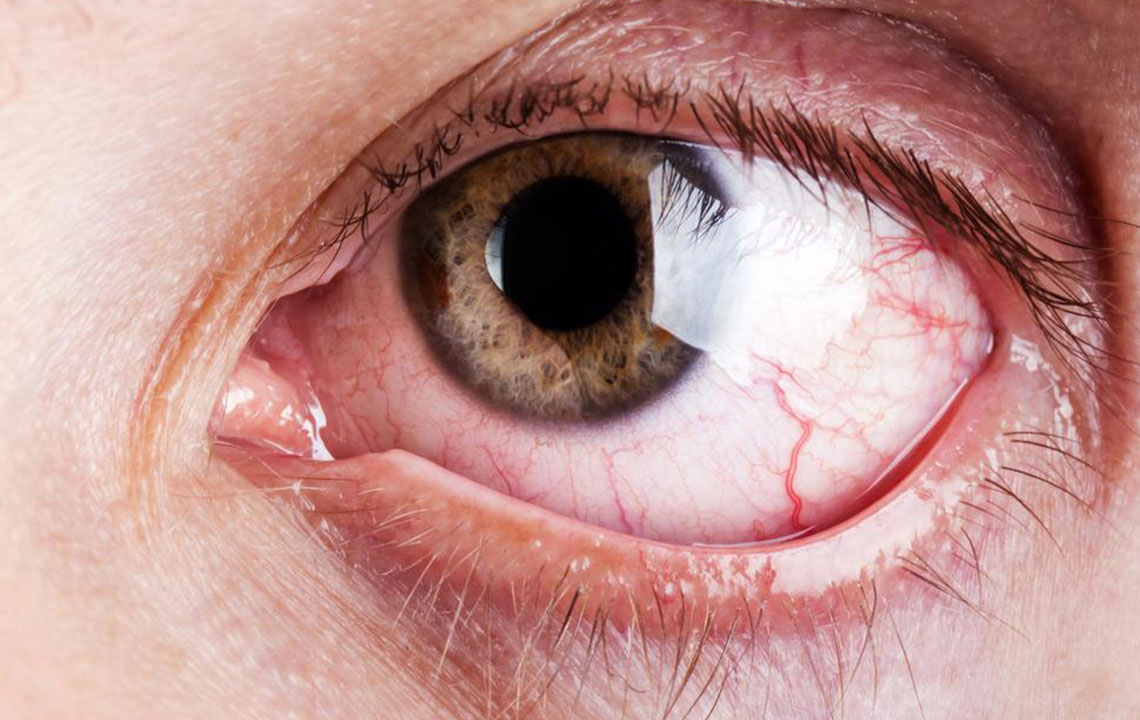
Dry eye syndrome, also known as keratoconjunctivitis sicca, affects millions worldwide, causing persistent discomfort, visual disturbances, and a significant decline in quality of life. This condition occurs when the eyes do not produce enough tears or when the tears evaporate too quickly, leaving the ocular surface dry and vulnerable to irritation. If you're experiencing symptoms like dryness, burning, itching, redness, or sensitivity to light, understanding the causes and exploring appropriate treatment options can greatly improve your eye health and comfort.
The human tear film is a complex mixture composed of three main layers: an oily outer layer that reduces evaporation, a watery middle layer that provides moisture and nutrients, and an inner mucous layer that helps spread tears evenly across the eye surface. When any of these components are disrupted, dry eye symptoms can develop. Factors such as aging, environmental conditions, certain medications, autoimmune diseases, and eyelid disorders can interfere with normal tear production and stability. Recognizing these causes is essential for effective management and tailored treatment plans.
Age is a significant risk factor, as tear production tends to decline with advancing years. Medications like antihistamines, decongestants, antidepressants, and blood pressure drugs can diminish tear secretion. Autoimmune conditions such as rheumatoid arthritis and Sjogren’s syndrome directly target tear and saliva-producing glands, resulting in severe dryness. Additionally, eyelid issues like blepharitis, meibomian gland dysfunction, or eyelid malpositions impact oil secretion, leading to faster tear evaporation. Environmental factors—including exposure to wind, smoke, dry climates, and prolonged screen time—further exacerbate dryness.
To diagnose dry eye syndrome accurately, ophthalmologists perform comprehensive eye examinations, including tear film assessments, slit-lamp evaluations, and testing tear volume through Schirmer’s test or tear breakup time analysis. These evaluations help determine the severity of dryness and guide appropriate treatment approaches.
Management strategies for dry eye syndrome are diverse and often personalized. Mild cases can often be managed with simple interventions, while severe cases may require more invasive procedures. The cornerstone of treatment involves lubricating eye drops, commonly known as artificial tears. These products mimic natural tears, relieving discomfort and protecting the ocular surface. Over-the-counter options include preservative-free drops, gels, and ointments, with thicker formulations used overnight to provide extended relief.
For persistent or more severe cases, specialized treatments aim to restore tear stability and improve gland function. Punctal plugs, inserted into the tear drainage pathways, prevent tears from draining away too quickly, thereby increasing ocular surface moisture. These plugs can be temporary dissolvable types or semi-permanent or permanent devices that require careful consideration and consultation with your ophthalmologist.
Another innovative treatment is LipiFlow, which employs controlled heat and pressure to unblock the meibomian glands responsible for secreting the oily layer of the tear film. Restoring their function helps reduce tear evaporation and stabilizes the tear film, offering significant relief for many patients. In cases where gland dysfunction is severe, gland expression or intense pulsed light therapy may be recommended.
In addition to mechanical and pharmaceutical treatment options, lifestyle changes play a vital role. Maintaining adequate hydration, using humidifiers in dry environments, taking regular breaks during screen use, and avoiding exposure to smoke or wind can significantly reduce symptoms. Nutritional support with omega-3 fatty acids, found in fish oils and flaxseed, has been shown to improve gland function and tear quality, providing a natural adjunct to conventional therapies.
In some circumstances, hormone therapy such as testosterone supplementation has been explored to improve gland function, especially in cases involving hormonal imbalances. However, such treatments should be carefully managed under medical supervision. Emerging therapies and continued research hold promise for more targeted and effective management of dry eye syndrome in the future.
In conclusion, dry eye syndrome is a multifaceted condition that requires a comprehensive approach to management. Early diagnosis and personalized treatment plans can effectively alleviate symptoms, restore eye comfort, and protect visual health. If you experience persistent dry, irritated, or gritty eyes, consult an eye care professional promptly to explore the best options tailored to your specific needs.