Comprehensive Guide to Detecting and Managing Low Blood Sugar Symptoms for Better Health
This comprehensive article explains the causes, symptoms, and management strategies for low blood sugar, emphasizing early detection and prompt response. It covers different severity levels, special cases like nighttime hypoglycemia, and prevention tips, aiming to empower individuals to handle hypoglycemia effectively and maintain their health. Essential for diabetics and caregivers, it highlights the importance of regular monitoring, emergency preparedness, and lifestyle adjustments for safe living.
Understanding and Managing Low Blood Sugar: A Complete Guide
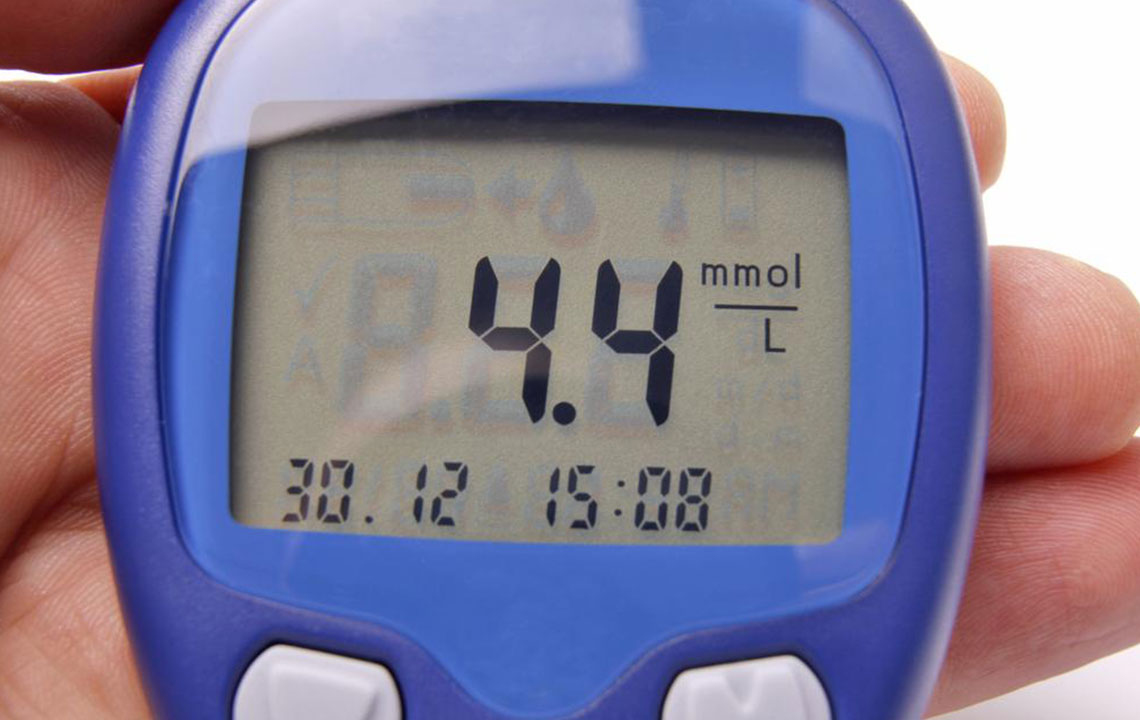
Low blood sugar, medically known as hypoglycemia, is a condition that occurs when blood glucose levels fall below normal ranges, typically under 70 mg/dL. Glucose serves as the primary source of energy for the body, powering vital organs and bodily functions. Maintaining balanced blood sugar levels is especially critical for individuals with diabetes, though hypoglycemia can affect anyone under certain circumstances. Recognizing the early signs and understanding how to respond effectively can prevent severe health consequences.
In this comprehensive guide, we'll explore the causes, symptoms, and management strategies for low blood sugar. Whether you're managing diabetes, supporting loved ones, or seeking to understand this condition better, understanding hypoglycemia is essential for safeguarding your health.
What Is Hypoglycemia and Why Does It Happen?
Hypoglycemia occurs when blood glucose levels drop below the normal threshold, often due to an imbalance between insulin, food intake, physical activity, or medication. It can happen to anyone but is most common among people with diabetes who use insulin or certain oral medications. Common causes include skipping meals, overeating without medication adjustment, excessive alcohol consumption, intense physical activity, or medication side effects. Recognizing these triggers helps in preventing episodes.
Recognizing the Symptoms of Low Blood Sugar
Symptoms of hypoglycemia can vary greatly depending on the severity of the blood glucose decline. Early signs are often subtle yet critical for early intervention. These include feelings of shakiness, sweating, irritability, hunger, rapid heartbeat, and dizziness. As blood sugar levels continue to decline, symptoms may progress to confusion, weakness, blurred vision, headaches, and difficulty concentrating. Severe hypoglycemia can lead to loss of consciousness, seizures, or coma if not treated promptly.
Understanding these symptoms allows individuals and caregivers to act swiftly, reducing the risk of dangerous complications. It's essential to monitor blood sugar levels regularly, especially if you experience symptoms or engage in activities that have the potential to cause fluctuations.
Daily Variations and Risk Factors
Blood sugar levels are subject to daily fluctuations influenced by meals, physical activity, stress, illness, and medication adherence. Athletes and active individuals should be particularly vigilant during and after exercise, as physical exertion can cause drops in glucose levels. Additionally, alcohol consumption can interfere with normal glucose regulation, leading to hypoglycemia, especially when consumed without adequate food intake.
Severity of Hypoglycemia and Its Clinical Signs
The severity of hypoglycemia can be classified into mild, moderate, and severe stages. Understanding these helps in determining the appropriate response.
Mild Hypoglycemia: Blood glucose levels under 70 mg/dL typically bring about symptoms like tremors, sweating, nervousness, nausea, and mild dizziness. These can often be corrected quickly by consuming fast-acting carbohydrates.
Moderate Hypoglycemia: When levels drop below 40 mg/dL, symptoms intensify. Individuals may experience confusion, difficulty focusing, irritability, slurred speech, and unsteady gait. Immediate action is crucial at this stage to prevent worsening.
Severe Hypoglycemia: Levels below 20 mg/dL pose significant danger, risking seizures, loss of consciousness, and potential death. Emergency medical intervention becomes necessary. Emergency kits containing glucagon and fast-absorbing carbs should always be available for high-risk individuals.
Special Considerations: Nighttime Hypoglycemia and Unawareness
Nighttime hypoglycemia presents unique challenges since symptoms occur during sleep, making detection harder. Signs include night sweats, restlessness, sleepwalking, nightmares, or waking with a headache. Proper nighttime monitoring and adjustments of medication or food intake can help prevent these episodes.
Hypoglycemic unawareness is a condition where individuals lose the ability to recognize warning symptoms, increasing the risk of sudden unconsciousness. Those affected should employ regular blood glucose monitoring and carry quick-acting carbohydrate supplies at all times. Educating oneself about managing these episodes is vital for safety.
Effective Prevention and Management Strategies
Prevention centers around routine blood sugar monitoring, especially before engaging in physical activity or meals. Maintaining a balanced diet with consistent carbohydrate intake and avoiding excessive alcohol consumption can significantly reduce risks. During hypoglycemic episodes, consuming approximately 15 grams of quick-absorbing carbs is recommended. Examples include glucose tablets, candies, fruit juices, honey, or soft drinks.
In cases of mild symptoms, promptly eating or drinking these sources can elevate blood sugar levels quickly. For severe episodes, emergency injection of glucagon or medical attention is necessary. Educating patients and caregivers on recognizing symptoms and administering appropriate treatment can save lives.
Emergency Response and When to Seek Medical Help
If someone shows signs of severe hypoglycemia, such as unconsciousness or seizures, immediate emergency services should be contacted. Do not attempt to give food or fluids to an unconscious person, as this can cause choking. Instead, administer glucagon if available, and position the person safely on their side while waiting for medical help to arrive.
Regular training for patients and caregivers on recognizing emergencies, using glucagon kits, and administering first aid can empower individuals to handle hypoglycemia effectively and prevent life-threatening complications.
Long-Term Management and Lifestyle Adjustments
Long-term management includes regular blood glucose monitoring, adhering to prescribed medication regimens, and maintaining a consistent eating and exercise schedule. Educating about carbohydrate counting and adjustments based on activity or illness can help in avoiding hypoglycemic episodes. Lifestyle modifications such as balanced nutrition, stress management, and avoiding excessive alcohol are also critical components.
Engaging with healthcare providers for personalized management plans and regular checkups ensures optimal control over blood sugar levels, reducing the risk of both hypoglycemia and hyperglycemia.
Conclusion: Stay Prepared for a Safer Life
Hypoglycemia remains a manageable condition with proper awareness, prevention, and timely response. Recognizing early symptoms, understanding severity levels, and having emergency supplies on hand are essential steps in ensuring safety. Whether you’re living with diabetes or caring for someone who is, staying vigilant and proactive makes a significant difference in maintaining a healthy and active life.
Keywords: low blood sugar, hypoglycemia symptoms, blood sugar management, emergency glucagon, diabetes safety





