Comprehensive Guide to Managing and Treating Leg Cellulitis Effectively
Leg cellulitis is a serious bacterial skin infection that demands prompt treatment to prevent severe complications. Effective management involves antibiotics, supportive care such as elevation and cold compresses, and immediate medical attention for worsening symptoms. Recognizing early signs and adhering to treatment plans are essential for full recovery. This comprehensive guide covers symptoms, treatment options, supportive measures, and prevention tips to help patients effectively manage leg cellulitis and avoid complications.

Comprehensive Strategies for Managing and Treating Leg Cellulitis
Leg cellulitis is a significant bacterial infection that affects the layers of skin and underlying tissues in the lower limbs. This condition manifests primarily through redness, swelling, warmth, and tenderness of the affected area. Although cellulitis itself is not contagious, it can pose serious health risks if not treated promptly and properly. Understanding how to manage and treat leg cellulitis effectively is vital to prevent its rapid progression and avoid potentially life-threatening complications.
Typically, cellulitis affects the lower legs, owing to the thinner skin and increased exposure to minor injuries or skin breaks in this region. Nevertheless, it can also occur on other parts of the body such as the arms, face, or torso. The common pathway for bacteria invasion is usually a small skin tear, cut, or insect bite that provides entry points for bacteria, especially if the skin's integrity is compromised. Once invading, the bacteria multiply rapidly, leading to inflammation and infection that, if left untreated, can spread swiftly to lymph nodes, bloodstream, and deeper tissues.
The causative agents of leg cellulitis are primarily bacteria, with Streptococcus and Staphylococcus species being the most common. These bacteria infiltrate the skin through minor injuries or skin conditions like eczema or dermatitis. Factors such as poor circulation, obesity, diabetes, immune deficiencies, or prior trauma increase susceptibility to cellulitis. In particular, individuals with compromised immune systems must be vigilant as the infection can escalate quickly into severe systemic illness.
Recognizing Symptoms and Signs of Leg Cellulitis
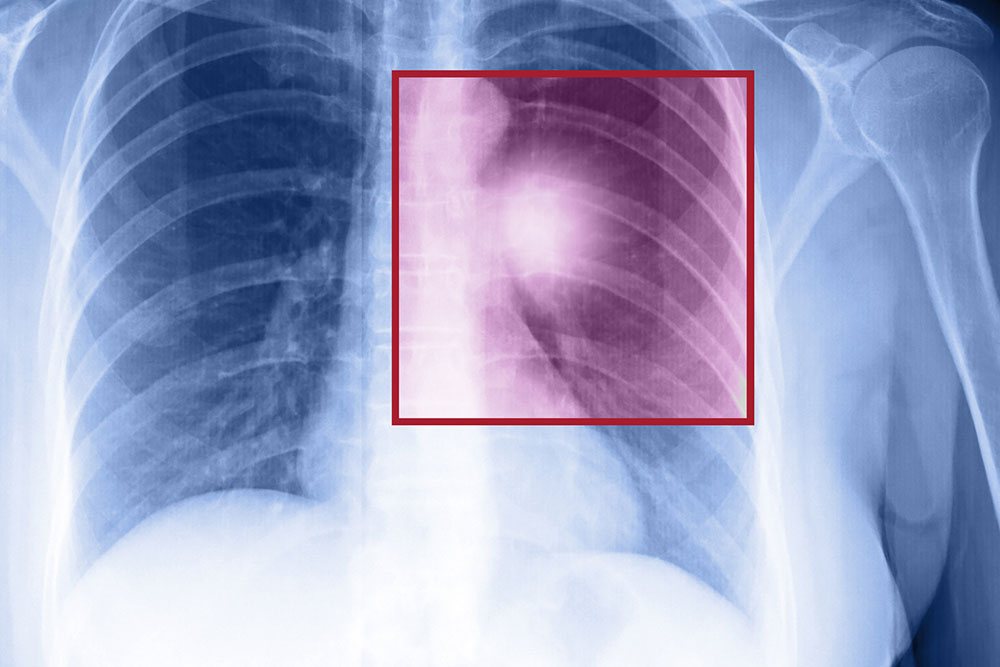
Early diagnosis plays a crucial role in the successful management of cellulitis. Typical symptoms include a visibly red, swollen, warm, and tender area on the skin. The redness often spreads gradually, and the skin may appear shiny and tight due to swelling. Accompanying symptoms may involve fever, chills, malaise, and in some cases, skin discoloration or spots. The infected area might also develop blisters or skin dimpling, indicating an advanced stage of infection. In severe cases, patients may experience high fever, chills, and lymph node swelling.
Effective Treatment Options for Leg Cellulitis
The cornerstone of cellulitis treatment involves prompt initiation of antibiotic therapy to eradicate the bacterial infection. Oral antibiotics are usually sufficient for uncomplicated cases, with effectiveness assessed within the first three days. The typical duration of treatment ranges from five to ten days, but in persistent or severe cases, the course may extend up to two weeks. It is imperative to complete the prescribed medication even if symptoms improve quickly, as stopping treatment prematurely can result in recurrent infection or antibiotic resistance.
In cases where symptoms are severe or do not respond to oral antibiotics, hospitalization with intravenous antibiotics might be necessary. This approach ensures higher antibiotic concentrations in the bloodstream, providing more aggressive treatment. It is essential to follow the healthcare provider's instructions closely and attend follow-up appointments to monitor progress and prevent complications.
Supporting Care and Home Remedies
Alongside antibiotic treatment, several supportive measures can facilitate recovery and relieve symptoms. Elevating the affected limb above heart level helps reduce swelling and promotes circulation. Applying cold compresses or ice packs can mitigate pain and decrease inflammation. Over-the-counter pain relievers like acetaminophen or NSAIDs are useful for managing discomfort. Wearing compression stockings can also aid in reducing swelling and improving blood flow. Maintaining good skin hygiene, keeping the skin clean and moisturized, helps prevent secondary infections.
Indicators of Critical Conditions and When to Seek Medical Help
While mild cellulitis can often be managed effectively at home under medical supervision, certain signs demand immediate medical attention. Watch for symptoms such as increasing redness, swelling, or warmth extending beyond the initial area, high fever, chills, general weakness, or the development of blisters, pus, or skin dimpling. These signs suggest worsening infection or systemic involvement, which requires urgent hospitalization for intravenous antibiotics and possibly surgical intervention. Prompt medical response is vital to prevent severe complications such as abscess formation, necrosis, or systemic sepsis.
Preventative measures include maintaining skin integrity by avoiding skin injuries, managing underlying health conditions like diabetes, and practicing good hygiene. If you recognize early signs of cellulitis or have risk factors, consulting a healthcare professional promptly can significantly improve outcomes and help prevent progression to serious health issues.