Comprehensive Guide to Dry Eye Disease: Causes, Symptoms, and Effective Management Strategies
Dry eye disease affects millions, especially older adults and women, causing discomfort and vision issues. This comprehensive guide covers its causes, symptoms, diagnosis, treatment options, and preventive strategies. Recognizing symptoms early and adopting lifestyle changes can greatly improve quality of life. From artificial tears to advanced therapies, effective management is attainable through a multi-pronged approach. Protect your eye health today by understanding this common but often overlooked condition.

Dry eye disease, medically known as keratoconjunctivitis sicca, is a prevalent condition that affects millions worldwide, particularly in developed countries. This condition manifests when the eyes do not produce sufficient tears or when tears evaporate too quickly, leading to a persistent sense of dryness and irritation. The impact of dry eye extends beyond mere discomfort; it can significantly impair vision quality and reduce overall quality of life. As the most common eye disorder, dry eye is especially prevalent among individuals over the age of 50, with women experiencing a higher incidence due to hormonal fluctuations during pregnancy, menopause, or hormone replacement therapy.
Understanding the Root Causes of Dry Eye Disease
The causes of dry eye are multifaceted, often involving a combination of factors that disrupt the delicate tear film essential for eye health. The tear film consists of three layers: oil, aqueous, and mucous, which work together to lubricate and protect the eyes. Disruption in any of these layers can lead to dry eye symptoms. Some primary causes include:
Aging: As we age, tear production naturally declines, making seniors more susceptible to dry eye.
Hormonal changes: Women undergoing hormonal fluctuations during pregnancy, menopause, or using hormone therapies tend to experience higher rates of dry eye due to changes in tear composition.
Environmental factors: Exposure to dry, windy, or smoky environments accelerates tear evaporation, leading to dryness.
Prolonged screen time: Excessive use of digital devices reduces blinking frequency, which decreases tear distribution across the eyes.
Underlying health conditions: Autoimmune disorders such as Sjögren’s syndrome, thyroid problems, allergies, and vitamin A deficiency significantly increase the risk of developing dry eye disease.
Medications: Certain medications including antihistamines, antidepressants, and blood pressure drugs can reduce tear production.
Recognizing the Symptoms of Dry Eye Disease
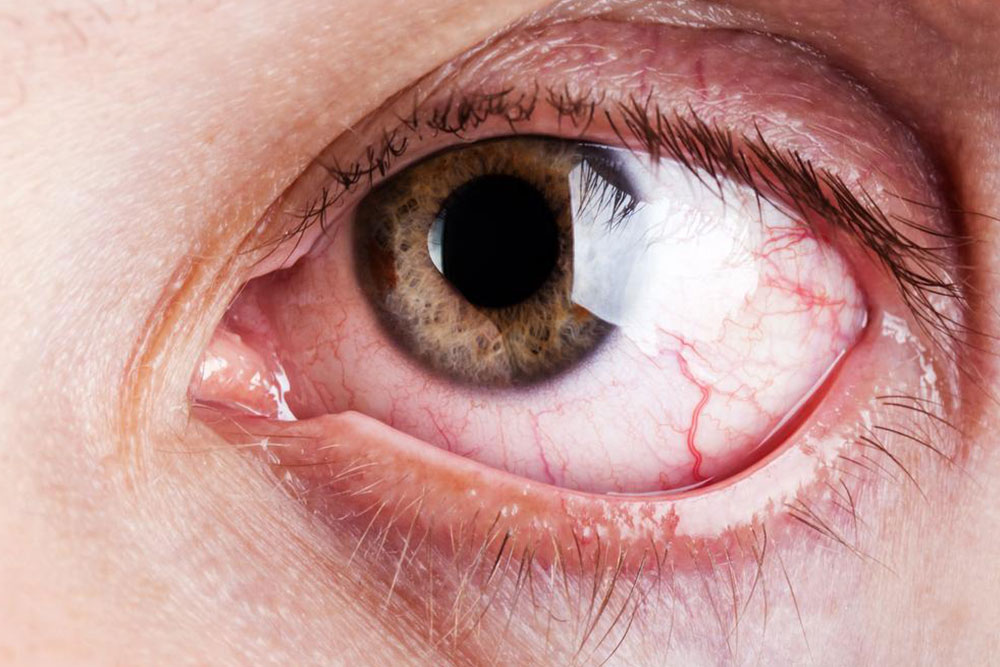
Recognizing the early symptoms of dry eye is essential for prompt treatment and prevention of complications. Common signs and symptoms include:
Persistent dryness and soreness: A constant feeling of dryness or grittiness in the eyes.
Redness and irritation: Eyes may appear red, inflamed, or swollen.
Burning or stinging sensation: Discomfort similar to a burning feeling often accompanies dryness.
Blurred or fluctuating vision: Vision may become unclear, especially after prolonged visual tasks.
Excessive tearing: Paradoxically, dry eye can stimulate reflex tearing as the eye tries to compensate.
Light sensitivity: Eyes become more sensitive to bright lights or glare.
Diagnosing Dry Eye Disease
Diagnosis involves a comprehensive eye examination performed by an ophthalmologist or optometrist. The clinician evaluates symptoms, conducts tear film assessments, and may perform tests such as the Schirmer test, tear breakup time (TBUT), and staining procedures to assess corneal damage or dryness extent. Early diagnosis allows for tailored treatment plans to address specific causes and severity.
Effective Treatment Options for Dry Eye
Managing dry eye disease involves a multifaceted approach aimed at alleviating symptoms and addressing underlying causes. Treatment strategies include:
Artificial tears and lubricating eye drops: Over-the-counter products provide immediate relief by supplementing natural tear film and protecting the eyes from irritation.
Prescription medications: Anti-inflammatory eye drops, such as cyclosporine (Restasis), can enhance tear production and reduce inflammation.
Addressing systemic causes: Managing autoimmune or hormonal conditions that contribute to dryness is crucial for long-term relief.
Environmental modifications: Using humidifiers, avoiding windy environments, and wearing wraparound glasses to shield eyes from dust and wind.
Meibomian gland dysfunction treatment: Techniques such as warm compresses, lid hygiene, and, in some cases, procedural interventions to improve oil layer quality and prevent tear evaporation.
Lifestyle adjustments: Reducing screen time, taking regular breaks during digital device use (the 20-20-20 rule), and maintaining proper eye hygiene can significantly improve symptoms.
Preventive Measures and Self-Care Tips
Prevention is better than cure when it comes to dry eye disease. Incorporating healthy habits can protect your eye health in the long run:
Protect your eyes from environmental stressors: Wear sunglasses or protective eyewear in windy or dusty conditions.
Limit screen time: Follow the 20-20-20 rule: every 20 minutes, look at something 20 feet away for at least 20 seconds.
Maintain indoor humidity: Use humidifiers to keep air moist, especially in winter or in air-conditioned rooms.
Stay hydrated and eat a balanced diet: Foods rich in omega-3 fatty acids, such as fish, flaxseeds, and walnuts, support healthy tear production.
Avoid smoking and exposure to smoke: Smoke can exacerbate dryness and irritate the eyes.
Practice good eyelid hygiene: Regular cleaning of eyelids can prevent the buildup of bacteria and debris that worsen dry eye symptoms.
When to Seek Medical Attention
If symptoms persist despite self-care measures, or if there is significant redness, pain, vision changes, or discharge, consult an eye care professional promptly. Chronic dry eye can lead to corneal abrasions, ulcers, and even vision loss if left untreated.
The Future of Dry Eye Treatment
Research continues to advance in understanding dry eye disease. Emerging therapies include biologic agents, innovative tear substitutes, new drug delivery systems, and laser-based treatments aimed at improving gland function. Personalized medicine approaches are being explored to tailor treatments based on individual cause profiles, improving efficacy and reducing side effects. Staying informed about new developments can help sufferers access more effective and targeted therapies in the future.
In conclusion, dry eye disease is a complex yet manageable condition. With early diagnosis, appropriate treatment, and lifestyle modifications, individuals can significantly reduce discomfort and protect their vision. Awareness of risk factors and adopting preventive habits are essential for maintaining optimal eye health in the long term.