In-Depth Guide to Managing and Treating Dry Eye Disease for Better Eye Health
Dry eye disease affects millions worldwide, causing discomfort and vision problems. This comprehensive guide covers causes, diagnosis, and treatment options, including lifestyle changes, medications, and advanced therapies. Early diagnosis and tailored management can significantly improve quality of life, prevent complications, and promote long-term eye health.

Comprehensive Insights into Dry Eye Disease: Causes, Diagnosis, and Treatment Strategies
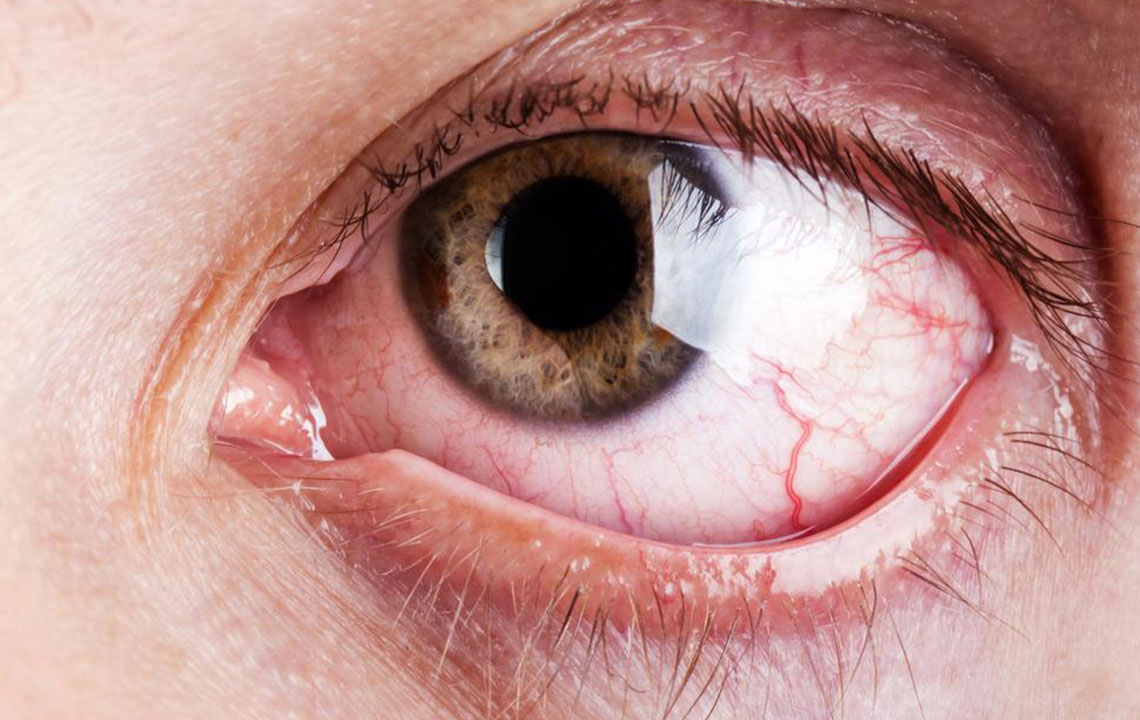
Dry eye disease (DED), also known as keratoconjunctivitis sicca, is a complex and prevalent condition affecting millions worldwide. It manifests as a persistent feeling of dryness, irritation, burning sensation, redness, blurred vision, and sometimes a gritty or foreign body sensation in the eyes. DED occurs when the eye’s tear production is insufficient or the quality of tears is compromised, leading to inadequate lubrication of the eye surface. This condition is particularly common among the elderly, especially those over 65, but it can also affect younger individuals due to various factors such as digital screen use, environmental conditions, medication use, or underlying health issues.
Understanding the root causes of dry eye disease is essential for effective management. It involves exploring the different types of DED, which include aqueous-deficient dry eye (caused by decreased tear production) and evaporative dry eye (caused by increased tear evaporation). Sometimes, individuals experience a combination of both. Factors like aging, hormonal changes, autoimmune disorders (like Sjögren’s syndrome), medications (antihistamines, antidepressants), contact lens wear, and environmental elements such as dry, windy, or air-conditioned environments can all contribute to the development of dry eye symptoms.
The Importance of Accurate Diagnosis
Diagnosing dry eye disease accurately is the cornerstone of successful treatment. Healthcare professionals employ a range of diagnostic tests, including evaluating tear volume via the Schirmer’s test, measuring tear film break-up time (TBUT), and analyzing the composition of tears for osmolarity. Additionally, a thorough medical history and physical examination of eyelids and corneal surfaces help identify contributing factors like eyelid margin abnormalities, meibomian gland dysfunction, or inflammation.
Advanced imaging techniques and tear film analysis provide further insights into tear stability and quality, enabling ophthalmologists to tailor treatment plans precisely. Proper diagnosis not only relieves symptoms but can also prevent the progression of the disease and potential damage to the ocular surface.
Effective Treatment Modalities for Dry Eye Disease
Managing dry eye disease requires a combination of lifestyle modifications, medical therapies, and sometimes surgical interventions. The primary goal is to restore a healthy tear film, reduce inflammation, and protect the ocular surface.
Artificial Tears and Lubricants
Over-the-counter artificial tears are often the first line of treatment. These eye drops supplement natural tears and provide immediate relief from dryness and irritation. They come in various formulations—preservative-free options are preferred for frequent use to avoid irritation.
Promoting Natural Tear Production
Medications such as cyclosporine eye drops (Restasis) and lifitegrast (Xiidra) help increase tear production by reducing inflammation and stimulating tear glands. For severe cases, procedures like punctal plugs—tiny devices inserted into tear ducts to block tear drainage—can conserve natural tears and improve eye moisture.
Addressing Underlying Causes
Treating eyelid conditions, such as blepharitis or meibomian gland dysfunction, is crucial. Warm compresses, eyelid scrubs, and antibiotics may be recommended. Correcting environmental factors—using humidifiers, avoiding smoke and wind, and taking regular breaks from digital screens—also reduces symptoms.
Emerging and Advanced Treatments
The field continues to evolve with innovative treatments like autologous serum eye drops, which use patients’ own blood serum as a tear substitute, and novel therapies that target inflammation more effectively. In some cases, intense pulsed light (IPL) therapy has shown promise for meibomian gland dysfunction, improving oil gland function and tear stability.
Preventive Strategies and Patient Education
Preventive care is vital, especially for individuals at high risk. Regular eye examinations, proper eyelid hygiene, adequate hydration, and environmental modifications aid in minimizing dry eye symptoms. Patient education about the importance of blinking regularly during screen time and avoiding known irritants enhances overall comfort.
When to Seek Medical Help
If you experience persistent dryness, discomfort, blurred vision, or if symptoms interfere with daily activities, consult an eye care professional promptly. Early intervention can prevent complications such as corneal abrasions or infections, which can result from severe dry eye.
In conclusion, dry eye disease is a multifaceted condition that requires personalized assessments and comprehensive management strategies. Advances in diagnostic techniques and treatment options provide hope for relief and improved quality of life. With proper care and lifestyle adjustments, individuals suffering from dry eye can achieve significant symptom relief and maintain healthy, functional eyes.