Comprehensive Guide to Pancreatitis: Recognizing Symptoms and Managing Complications
This comprehensive guide explores pancreatitis, covering its causes, symptoms, and potential complications. Early diagnosis and proper management are essential to prevent serious health issues such as infections, breathing problems, and diabetes. The article provides insights into recognizing symptoms like abdominal pain and nausea and highlights preventive measures to maintain pancreatic health. Suitable for individuals at risk or experiencing symptoms, this detailed overview aims to inform and promote proactive healthcare actions to safeguard overall well-being.

Comprehensive Guide to Pancreatitis: Recognizing Symptoms and Managing Complications
Pancreatitis is a serious medical condition characterized by inflammation of the pancreas, a critical organ located deep within the upper abdomen behind the stomach. The pancreas plays an essential role in digestion by producing enzymes that help break down food, and it also regulates blood sugar levels through insulin secretion. Understanding the nature of pancreatitis, its symptoms, possible complications, and when to seek medical attention is vital for effective management and prevention of severe health issues.
The condition can manifest as either acute or chronic forms. Acute pancreatitis typically develops suddenly and lasts for a short period, usually resolving within days to weeks with appropriate treatment. Chronic pancreatitis, on the other hand, develops gradually over time, often resulting from persistent inflammation, and may lead to long-term damage to the pancreas. Recognizing the early signs, such as persistent abdominal pain, nausea, and fever, is crucial in seeking timely medical intervention to minimize potential complications.
Understanding the Causes and Risk Factors of Pancreatitis
The causes of pancreatitis are diverse, with common factors including gallstones, chronic alcohol consumption, certain medications, genetic predispositions, and high triglyceride levels. Gallstones can obstruct the pancreatic duct, leading to inflammation, while excessive alcohol intake damages pancreatic tissue over time. Additionally, metabolic disorders like hypertriglyceridemia and inherited genetic conditions can predispose individuals to develop this condition.
Recognizing the Symptoms Early
Early detection of pancreatitis relies on identifying its hallmark symptoms. These include:
Severe Upper Abdominal Pain: Often sudden, persistent, and may radiate to the back or shoulders.
Nausea and Vomiting: Common accompanying symptoms that can exacerbate dehydration and malnutrition.
Fever and Elevated Heart Rate: Indicators of systemic inflammation or infection.
Digestive Issues: Such as bloating, indigestion, and weight loss in chronic cases.
If untreated, these symptoms can worsen and lead to serious complications. Immediate medical consultation is advised when experiencing persistent abdominal pain or other related symptoms.
Potential Complications of Severe Pancreatitis
Severe pancreatitis can lead to numerous critical health problems, including:
Infections: Inflamed pancreatic tissue becomes vulnerable to bacterial or viral invasion, which can result in abscess formation requiring surgical intervention.
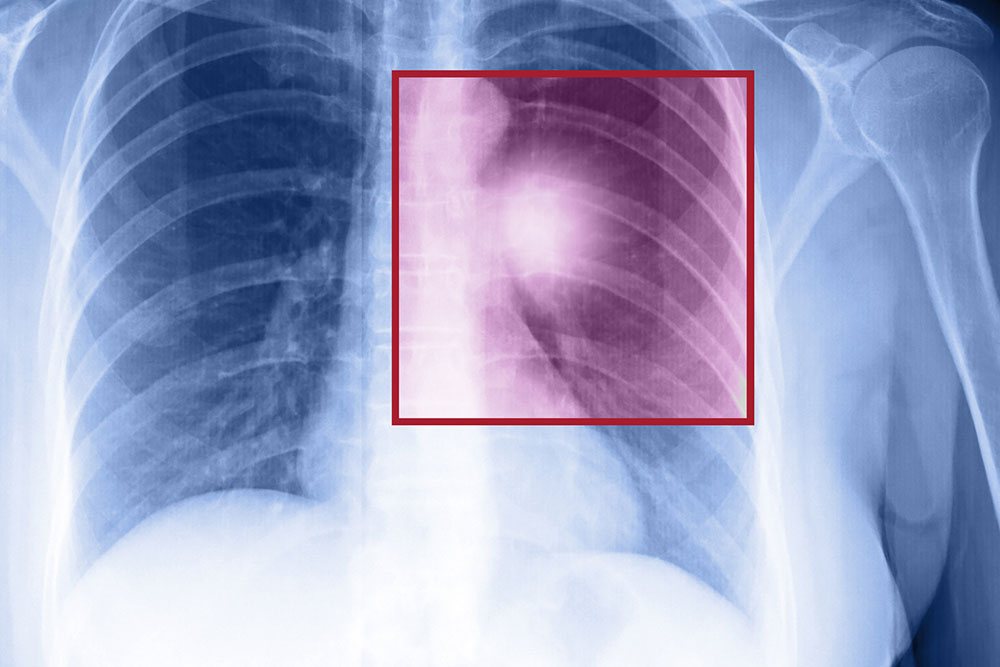
Respiratory Issues: The inflammation may spread or induce systemic responses that impair lung function, leading to breathing difficulties and low oxygen levels.
Development of Diabetes: Damage to the insulin-producing cells in the pancreas may cause impaired glucose regulation, eventually resulting in diabetes mellitus.
Nutritional Deficiencies: Reduced production of digestive enzymes hampers the breakdown and absorption of nutrients, leading to malnutrition, weight loss, and vitamin deficiencies.
Organ Failure: In extreme cases, unchecked inflammation can affect other organs, such as the kidneys and heart, increasing life-threatening risks.
Diagnosis and Treatment Strategies
Diagnosing pancreatitis involves blood tests, imaging scans like ultrasound or CT, and sometimes, endoscopic procedures. Early diagnosis is critical to preventing the progression of the disease. Treatment typically includes fasting to rest the pancreas, hydration, pain management, and addressing underlying causes like gallstones or alcohol use. Severe cases might require hospitalization, antibiotics, or even surgical procedures to remove damaged tissue or drain abscesses.
Preventive Measures and Lifestyle Modifications
Preventive strategies focus on managing risk factors by adopting a healthy lifestyle. Key measures include maintaining a balanced diet low in fats, avoiding excessive alcohol consumption, managing triglyceride levels, and seeking medical advice for any metabolic disorders. Regular medical checkups can help detect early signs of pancreatic issues, especially in high-risk individuals with familial predispositions or predisposing conditions.
When to Seek Medical Help
If you experience persistent upper abdominal pain, unexplained weight loss, fever, nausea, or vomiting, it is essential to seek prompt medical attention. Early intervention can significantly improve outcomes and reduce the risk of severe complications. Maintaining awareness of the symptoms and risk factors associated with pancreatitis is crucial for timely diagnosis and effective treatment.
In conclusion, pancreatitis is a complex condition with potentially serious consequences if not diagnosed and managed promptly. Staying vigilant about symptoms and understanding the associated risks can greatly enhance outcomes and quality of life for affected individuals. Consulting healthcare professionals at the first sign of trouble is the best course of action to prevent complications and preserve pancreatic function.