Comprehensive Guide to the Top 10 Factors Increasing Myeloma Risk and Prevention Strategies
This comprehensive article explores the top 10 risk factors for myeloma, including age, genetics, environmental exposures, and lifestyle influences. It provides insights into early detection and prevention strategies, emphasizing the importance of awareness for high-risk groups. Learn how understanding these factors can aid in timely diagnosis and improve treatment outcomes for this complex blood cancer.

Bone marrow is a vital soft tissue found within our bones that plays an essential role in producing the blood components necessary for our health. It creates red blood cells responsible for oxygen delivery, white blood cells that support our immune system, and platelets that aid in blood clotting. However, certain disorders can affect bone marrow, and one such critical condition is multiple myeloma—a complex type of blood cancer that originates from plasma cells, a specialized subset of white blood cells tasked with producing antibodies to combat infections.
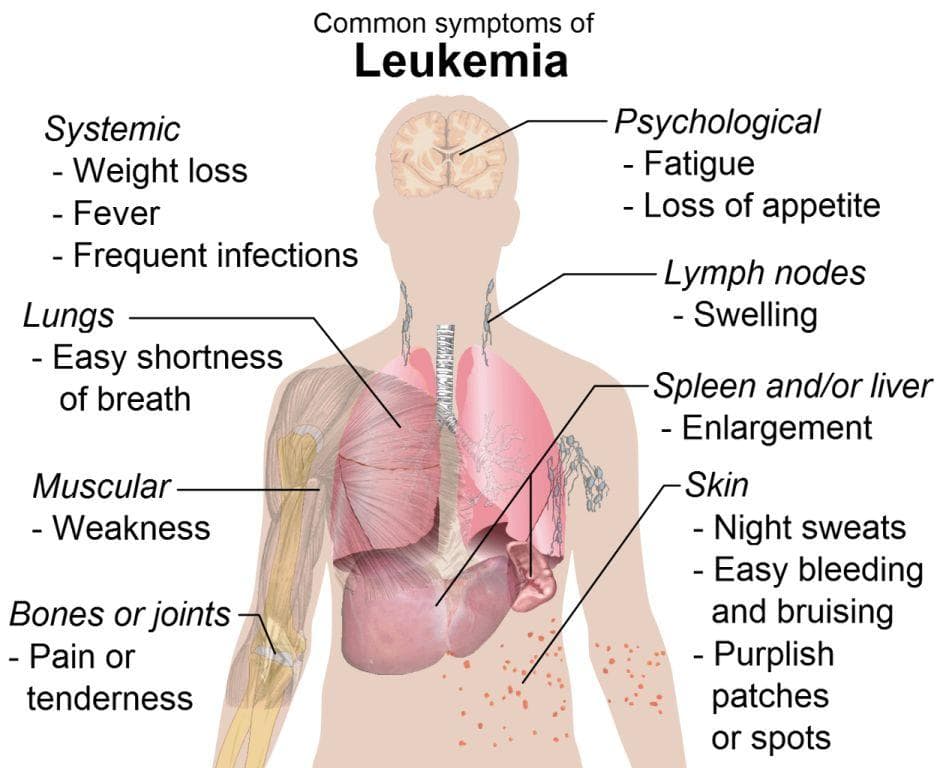
In the case of myeloma, abnormal plasma cells proliferate uncontrollably within the bone marrow. This unchecked growth can crowd out healthy blood cells, leading to a range of serious health issues. Patients often experience anemia due to decreased red blood cell production, increased susceptibility to infections owing to impaired white blood cell function, and bleeding problems resulting from low platelet counts. Additionally, these rogue plasma cells release abnormal proteins that can cause kidney damage. The excess growth of malignant cells also damages bones, leading to pain, bone fractures, and osteoporosis-like symptoms.
The exact etiology—or cause—of myeloma remains largely elusive. Scientists believe that a combination of genetic factors, environmental exposures, and lifestyle choices contribute to its development. Understanding these risk factors is crucial for early detection, intervention, and possibly prevention. Let’s explore the top 10 factors associated with an increased risk of developing myeloma, along with strategies for awareness and early diagnosis.
Top 10 Factors That Elevate the Risk of Developing Myeloma
Age: The risk of myeloma significantly increases with age, predominantly affecting older adults. Most cases are diagnosed between the ages of 60 and 65, owing to age-related genetic mutations and cumulative exposure to risk factors over time. As the body's cellular processes slow down and DNA repair mechanisms weaken, the likelihood of abnormal plasma cell growth rises, making age the most prominent risk factor for myeloma.
Ethnicity and Race: Ethnicity plays a substantial role in myeloma susceptibility. Studies have shown that African-Americans are approximately twice as likely to develop myeloma compared to Caucasians and Asians. The reasons behind this disparity may involve genetic predispositions, socio-economic factors, and environmental exposures prevalent within certain communities. Awareness of these racial disparities can lead to targeted screening and early detection programs in high-risk populations.
Gender: Men are statistically more vulnerable to myeloma than women. Several theories suggest hormonal differences and genetic factors may contribute to this gender disparity. Recognizing this pattern can help healthcare providers identify at-risk groups and tailor screening recommendations accordingly.
Monoclonal Gammopathy of Unknown Significance (MGUS): MGUS is a benign condition characterized by the presence of abnormal monoclonal proteins in the blood. While MGUS itself does not cause symptoms or health problems, it serves as a precursor condition that increases the likelihood of progressing to myeloma or related plasma cell disorders. Regular monitoring of MGUS patients is crucial for early intervention and disease management.
Family History: A documented family history of myeloma or other plasma cell disorders significantly elevates individual risk. Genetic predisposition plays a pivotal role, suggesting that inherited genes influence susceptibility. Individuals with a strong family history should consider genetic counseling and routine screenings for early detection.
Environmental Exposures: Exposure to harmful environmental agents such as ionizing radiation, pesticides, certain fertilizers, and chemicals like Agent Orange has been linked to increased myeloma risk. Agricultural workers, veterans, and individuals working with hazardous substances should take appropriate protective measures and undergo regular health screenings.
Immunosuppressive Treatments: Patients who undergo immunosuppressive therapies post-organ transplantation or for autoimmune diseases face an increased risk. Suppressed immune function hampers the body's ability to detect and eliminate abnormal plasma cells, raising the risk of malignancy. Regular blood tests and surveillance can aid in early diagnosis in high-risk groups.
Autoimmune Diseases: Conditions such as ankylosing spondylitis, autoimmune hemolytic anemia, and systemic lupus erythematosus have been identified as potential risk factors. The chronic immune activation in these diseases may promote abnormal plasma cell proliferation, thereby increasing myeloma risk.
Gaucher Disease: As a genetic disorder marked by the abnormal accumulation of fatty substances in organs, Gaucher disease has been associated with an elevated risk of plasma cell dyscrasias, including myeloma. Patients with Gaucher should be vigilant and undergo periodic assessments for early signs of hematologic malignancies.
Obesity: Excess body weight is a significant modifiable risk factor for myeloma. Obesity is associated with chronic inflammation, alterations in immune function, and hormonal imbalances, all of which can contribute to plasma cell abnormalities. Adopting a healthy lifestyle, including diet and exercise, can reduce the risk of myeloma and other metabolic disorders.
Understanding the Risks and Taking Preventive Measures
While not all risk factors are modifiable, awareness of these key elements enables individuals and healthcare providers to take proactive steps for early detection and prevention. For example, high-risk populations—such as older adults, individuals with a family history, or those exposed to hazardous chemicals—should consider routine screening for monoclonal proteins or other early markers of disease.
Regular medical check-ups are vital, especially if you belong to a high-risk group. Blood tests to monitor for abnormal proteins, bone scans, and other diagnostic tools can facilitate early diagnosis, improving treatment outcomes. Lifestyle changes, such as maintaining a healthy weight, minimizing exposure to environmental toxins, and managing autoimmune conditions with medical guidance, can help mitigate the risk.
Researchers continue to explore the underlying genetic, environmental, and lifestyle factors contributing to myeloma. Advances in personalized medicine and targeted therapies also enhance the prospects for early detection and effective treatment options, ultimately improving patient survival and quality of life.
Summary
Myeloma is a complex hematological malignancy with multiple risk factors ranging from age and ethnicity to environmental exposures and genetic predispositions. By understanding these factors, individuals can make informed decisions about screening and lifestyle choices. Early detection remains crucial for successful management and improved prognosis. If you suspect you have risk factors or experience symptoms such as bone pain, fatigue, or recurrent infections, seek medical attention promptly. Staying informed and vigilant is the key to combating this challenging disease.