Medical Conditions That Significantly Contribute to Osteoporosis and Bone Weakness
This comprehensive guide explores medical conditions that accelerate osteoporosis and weaken bones. It highlights autoimmune diseases, diabetes, asthma medications, and thyroid disorders as significant contributors. Understanding these associations assists in early detection and preventive strategies, helping reduce fracture risk and improve quality of life for those vulnerable to bone loss. Learn about how health issues impact bone density and what steps can be taken to maintain strong, healthy bones over time.
Understanding How Certain Health Conditions Accelerate Osteoporosis and Bone Fragility
Osteoporosis, a condition characterized by fragile bones, is often linked to various medical conditions that hasten bone loss. Recognizing these health issues can play a vital role in prevention and management.
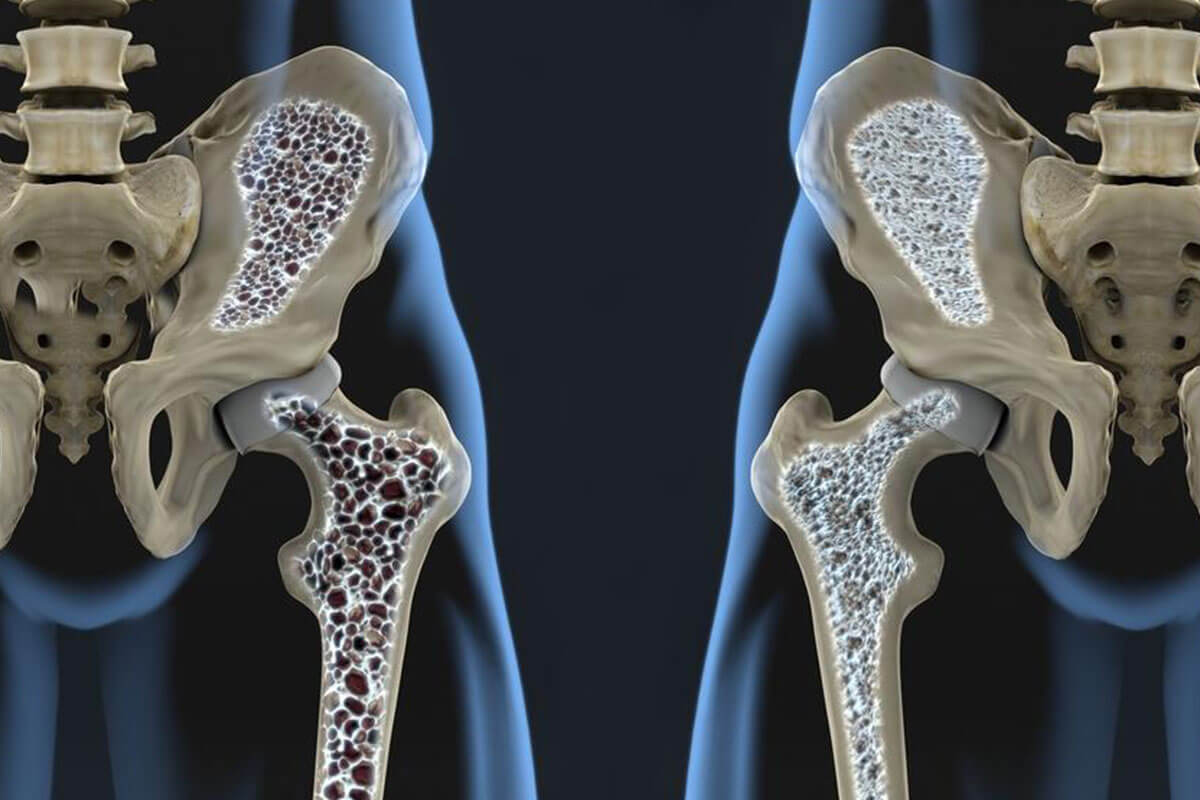
Bones are remarkable living tissues that serve vital functions, including structural support, protection of vital organs, and mineral storage. Their continual renewal process involves a balance between bone formation and resorption. When this balance tips in favor of breakdown, bones become weaker, leading to osteoporosis—a silent but serious disease affecting millions worldwide. Although it can affect individuals of any age or background, osteoporosis is especially prevalent among women, with estimates suggesting that over 200 million women globally have this condition. Women, particularly postmenopausal women, are at higher risk due to hormonal changes that influence bone density. However, men can also develop osteoporosis, especially with advancing age or certain health issues.
As osteoporosis advances, the risk of fractures dramatically increases. Fragile bones may fracture even from minor stresses like bending, coughing, or slipping. Common fracture locations include the spine, hips, and wrists. Sometimes early osteoporosis presents no symptoms, making early diagnosis challenging. Over time, signs such as gradual height loss, persistent back or neck pain, fractures, and a stooped posture may appear. A simple bone density scan, a non-invasive diagnostic tool, can identify the severity of bone loss and help formulate effective treatment plans.
Numerous factors influence osteoporosis risk, including individual body structure, age, genetics, race, lifestyle factors such as smoking and alcohol consumption, gender, and overall nutritional health. Managing risk involves a combination of medication, lifestyle changes, and dietary adjustments tailored to each person's unique health profile and fracture risk level. Preventive strategies are crucial because osteoporosis-related fractures can significantly impair quality of life and increase mortality risk, especially among the elderly.
What exactly causes osteoporosis bone loss? While the precise etiology remains complex and not completely understood, several medical conditions and their treatments can adversely affect bone health. Understanding these associations allows for targeted preventative measures and early interventions.
Rheumatoid Arthritis (RA) and Lupus
Autoimmune diseases like rheumatoid arthritis (RA) and systemic lupus erythematosus (commonly called lupus) involve the immune system erroneously attacking the body's own tissues. These chronic conditions affect millions — approximately 3 million adults in the United States alone. Lupus particularly tends to affect women aged 15 to 45, coinciding with peak bone development years, which heightens osteoporosis risk. According to Dr. Beatrice Edwards from Northwestern University, "Any disruption or interference with normal bone growth during these critical years can significantly elevate the chances of developing osteoporosis later in life." Both RA and lupus contribute to accelerated bone loss through inflammation and the side effects of medications used for treatment, such as corticosteroids.
Diabetes
Diabetes, especially type 1, has been linked to compromised bone health. Research suggests that the high blood sugar levels characteristic of diabetes can hinder the formation of new bone tissue, resulting in a lower peak bone mass. Dr. Edwards explains, "Type 1 diabetes often develops during childhood, a crucial period for achieving optimal peak bone mass. If this process is hindered, the risk of osteoporosis increases significantly as individuals age." Additionally, some diabetic medications may have adverse effects on bone density, further complicating bone health management.
Asthma
Asthma itself does not directly cause bone loss. However, treatments commonly used to manage asthma—particularly corticosteroids—are notorious for their side effects on bones. Long-term use of these anti-inflammatory drugs can lead to decreased bone mineral density, increasing fracture risk over time. While corticosteroids are effective in controlling asthma symptoms, they require careful monitoring and alternatives should be considered to minimize bone health risks.
Overactive Thyroid (Hyperthyroidism)
Hyperthyroidism, characterized by excessive thyroid hormone production, speeds up the body's metabolic processes—including bone remodeling cycles. After the age of 30, bone remodeling becomes less efficient, and increased activity cycles can lead to net bone loss. Dr. Edwards notes, "More frequent bone turnover cycles mean more opportunities for bone to be resorbed faster than it is formed, gradually weakening the skeleton." Managing hyperthyroidism effectively can mitigate its impact on bones.
Other medical conditions associated with increased osteoporosis risk include multiple sclerosis, celiac disease, and certain hormonal disorders. Recognizing these links enables clinicians and patients to adopt proactive strategies, such as vitamin D supplementation, calcium intake, lifestyle modifications, and appropriate medical treatments, all aiming to protect and preserve bone health throughout life.