Comprehensive Overview of Medical Conditions That Accelerate Osteoporosis and Bone Weakening
Osteoporosis is a silent disease that weakens bones, increasing fracture risk. Several medical conditions, including autoimmune diseases like rheumatoid arthritis and lupus, metabolic disorders such as diabetes, and hormone imbalances like hyperthyroidism, significantly contribute to bone loss. Long-term medication use, especially corticosteroids, further aggravates the condition. Early detection through bone density tests and proactive management—like lifestyle changes, medications, and nutritional support—are vital to prevent severe fractures. Understanding these medical links enables better prevention and treatment strategies to maintain strong, healthy bones throughout life.

Comprehensive Overview of Medical Conditions That Accelerate Osteoporosis and Bone Weakening
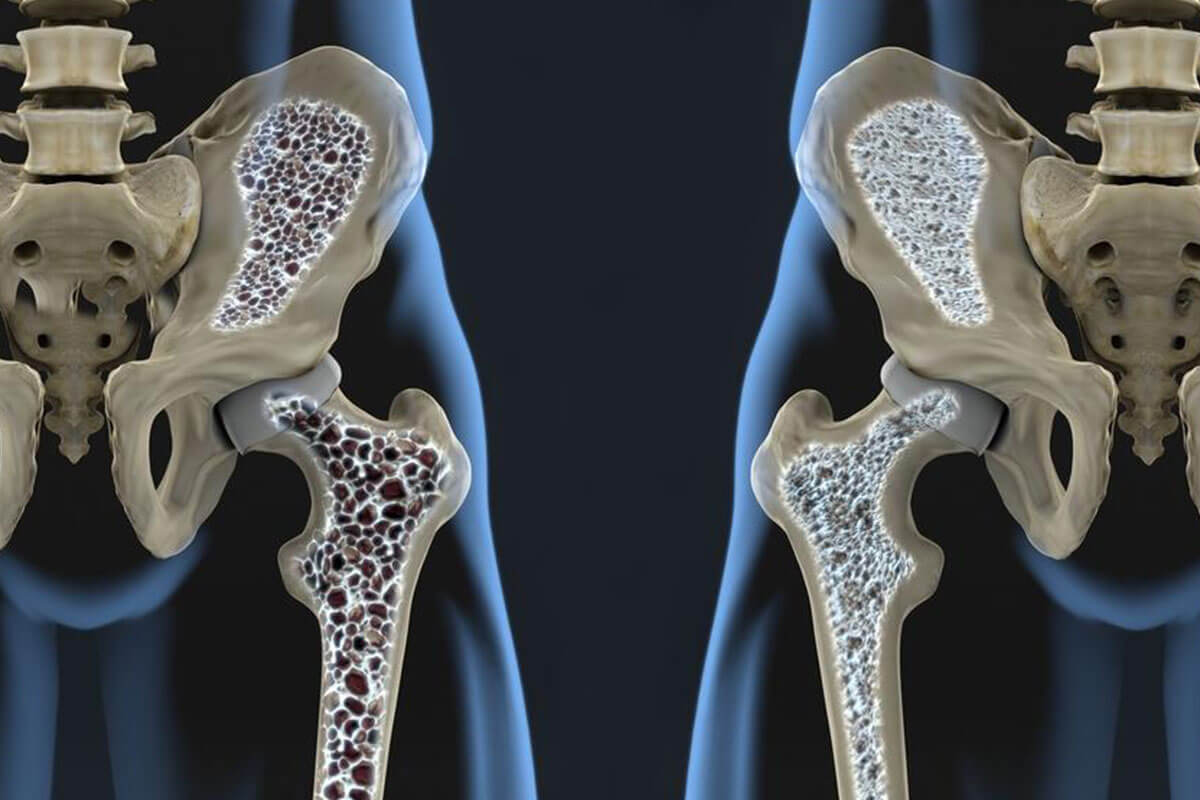
Osteoporosis is a widespread skeletal disorder characterized by decreased bone density and deterioration of bone tissue structure, leading to increased fragility and susceptibility to fractures. This condition silently progresses over time, often remaining undetected until a fracture occurs, making understanding its contributing factors crucial for effective prevention and management. Among these factors, certain medical conditions significantly influence the progression of osteoporosis by either directly impairing bone health or through the side effects of their treatments.
Bone is a dynamic tissue that undergoes constant remodeling—a balanced process of bone formation and resorption. When this balance is disturbed, particularly when bone breakdown exceeds formation, bones become porous, weak, and more likely to fracture under minor stress or falls. Globally, more than 200 million women are affected by osteoporosis, especially those over the age of 50. The prevalence is notably higher among white and Asian populations due to genetic and lifestyle factors. The most common fracture sites include the spine, hips, and wrists, which often occur after seemingly minor incidents such as falling from standing height, even during daily activities. Early diagnosis through bone density scans is vital for intervention, as symptoms like gradual height loss, back pain, and stooped posture typically emerge in advanced stages.
Age, gender, racial background, and lifestyle choices play significant roles in determining individual risk levels.
Adequate prevention involves use of osteoporosis medications when necessary, lifestyle modifications, nutritional adjustments, and regular screening.
The causes of osteoporosis are complex and multifactorial. Certain medical conditions substantially contribute to bone degradation either by directly affecting bone metabolism or through medication side effects. Being aware of these conditions enables healthcare providers and patients alike to take preventive steps, such as timely vitamin D and calcium supplementation, lifestyle changes, or targeted treatments to mitigate bone loss.
Autoimmune Diseases: Rheumatoid Arthritis and Systemic Lupus Erythematosus
Autoimmune disorders, especially rheumatoid arthritis (RA) and lupus (systemic lupus erythematosus), involve an abnormal immune response where the body's immune system mistakenly attacks its tissues, including bones. Chronic inflammation associated with these diseases hampers osteoblast activity (cells responsible for building bone) and accelerates osteoclast activity (cells that break down bone), resulting in net bone loss. In women aged between 15 and 45, these conditions can interfere with peak bone mass development, increasing the likelihood of osteoporosis in later life. Effective disease management and anti-inflammatory therapies are essential to preserve bone strength in affected individuals.
Diabetes Mellitus
Type 1 diabetes, usually diagnosed during childhood or adolescence, is characterized by insulin deficiency. Elevated blood sugar levels interfere with normal bone remodeling, impairing osteoblast function and leading to decreased bone formation. Over time, this metabolic disturbance can prevent achieving optimal bone density, setting the stage for osteoporosis in later years. Additionally, poor glycemic control in diabetes patients can predispose to other complications, including increased fracture risk due to higher fall propensity and delayed healing.
Asthma and Long-Term Use of Corticosteroids
While asthma itself is not directly linked to osteoporosis, management often necessitates the use of corticosteroids such as prednisone. Prolonged use of these medications, especially at high doses, markedly weakens bone tissue by decreasing osteoblast activity and increasing osteoclast-mediated resorption. This side effect significantly elevates osteoporosis risk among long-term corticosteroid users, particularly in older adults. Monitoring bone density and implementing preventive strategies like calcium and vitamin D supplementation are recommended for patients on chronic corticosteroids.
Hyperthyroidism
Overproduction of thyroid hormones in hyperthyroidism accelerates the body's metabolic processes, including bone turnover. The increased rate of bone resorption surpasses bone formation, leading to net bone loss. This effect becomes more pronounced after the age of 30, when bone remodeling efficiency declines naturally. Adequate treatment of hyperthyroid states can mitigate bone loss; however, if left uncontrolled, it can contribute significantly to osteoporosis development.
Other associated medical conditions that may influence bone health include multiple sclerosis, which impairs mobility and balance increasing fall risk, and celiac disease, which affects nutrient absorption, leading to deficiencies in calcium and vitamin D. Recognizing these links allows clinicians to implement strategies such as nutritional supplementation, disease control, and lifestyle counseling to safeguard bone health and prevent osteoporosis progression.