Comprehensive Guide to Syphilis: Symptoms, Stages, and Prevention
This comprehensive guide explains syphilis, covering its symptoms, stages, diagnosis, and prevention. It emphasizes the importance of early detection for effective treatment and highlights risk factors associated with this infectious disease. The article aims to raise awareness and promote preventive measures to curb its spread.
Comprehensive Guide to Syphilis: Symptoms, Stages, and Prevention
Syphilis remains a significant public health concern worldwide, despite being one of the oldest known sexually transmitted infections (STIs). Caused by the bacterium Treponema pallidum, syphilis can present a wide range of symptoms that vary across different stages of infection. While the global incidence declined sharply in the early 2000s, recent years have shown an unsettling resurgence, highlighting the importance of awareness, early detection, and effective treatment. In this comprehensive overview, we will explore the various stages of syphilis, their associated symptoms, methods for diagnosis, risk factors, and steps for prevention.
Understanding the Stages of Syphilis Syphilis is characterized by multiple stages—primary, secondary, latent, and tertiary—and each stage has distinct clinical features. Recognizing these signs early can make a significant difference in treatment outcomes and prevent long-term health complications.
Primary Stage: The Initial Signs The primary stage occurs approximately 2 to 12 weeks after exposure to infected bodily fluids. The hallmark sign is a painless, firm sore called a chancre, which typically develops on the genitals, anus, or mouth. This sore can easily be mistaken for other skin lesions or trauma, which often leads to delayed diagnosis. Chancres generally heal within 3 to 6 weeks without treatment, but the infection remains dormant and can progress to subsequent stages if not properly addressed. Swollen lymph nodes may also be present near the site of the sore, serving as an early indicator of infection. Since the primary lesion is often painless and heals on its own, many individuals might remain unaware of the infection during this stage.
Secondary Stage: Widespread Symptoms A few weeks after the primary sore heals, some individuals experience the secondary stage. This stage is marked by systemic symptoms that can affect various parts of the body. A typical sign is a non-itchy rash, often appearing on the palms of the hands and soles of the feet, but it can also spread to other areas. These rashes may be accompanied by mucous patches, which are moist, flat, wart-like lesions in the mouth, throat, or genital areas. Other symptoms include fatigue, fever, sore throat, headaches, muscle aches, and hair loss. Swollen lymph nodes are common during this phase. Because symptoms can mimic other illnesses, secondary syphilis often goes undiagnosed unless specific testing is performed. This stage is highly contagious due to the widespread nature of the skin lesions and rashes.
Latent and Tertiary Stages: Hidden Dangers If untreated, the infection can enter a latent period, which may last for months or even years. During this phase, there are no visible symptoms, but the bacterium remains in the body, silently causing damage. Many individuals in the latent stage might remain symptom-free indefinitely, yet the infection continues to pose health risks. After several years, some untreated individuals progress to tertiary syphilis, which can lead to severe and potentially life-threatening complications. Tertiary syphilis can affect multiple organ systems, resulting in neurological issues like general paresis or tabes dorsalis, cardiovascular problems such as aneurysms or aortitis, and extensive skin gummas—debilitating lesions that can cause tissue destruction.
Congenital Syphilis: Infection from Mother to Child Syphilis can be transmitted from an infected pregnant woman to her fetus through the placenta or during childbirth. Congenital syphilis manifests in newborns with symptoms like skin sores, jaundice, anemia, enlarged liver and spleen, nasal discharge (snuffles), and bone abnormalities. Without prompt treatment, affected infants may suffer from deafness, dental deformities, neurological deficits, and developmental delays. Congenital syphilis can also cause premature birth or stillbirth, emphasizing the need for early prenatal screening and treatment of expectant mothers.
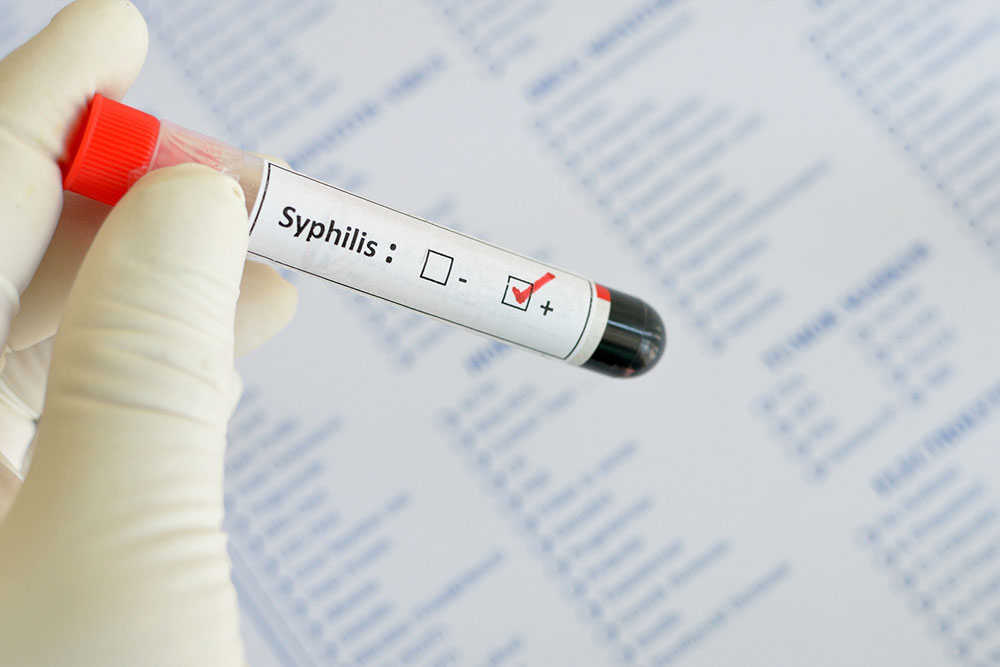
Diagnosing Syphilis: Laboratory Tests and Examination Accurate diagnosis of syphilis relies on a combination of clinical assessment and laboratory testing. Healthcare providers typically begin with detailed patient history-taking and physical examination. Blood tests are the cornerstone of syphilis diagnosis, including non-treponemal tests such as the Rapid Plasma Reagin (RPR) or Venereal Disease Research Laboratory (VDRL), which are useful for initial screening. Confirmatory testing involves treponemal tests like the Treponema pallidum Particle Agglutination (TP-PA) assay or fluorescent treponemal antibody absorption (FTA-ABS) test to verify infection. In cases involving infants or pregnant women, additional diagnostic procedures—such as microscopy of lesions, PCR (polymerase chain reaction), or cerebrospinal fluid analysis—may be necessary. Early detection is critical in managing syphilis effectively, preventing progression to more severe stages, and reducing transmission risk.
Risk Factors and Prevention Strategies Certain groups are at higher risk of contracting syphilis. These include individuals engaging in unprotected sexual activity, men who have sex with men, people living with HIV, and those with multiple sexual partners. Having other sexually transmitted infections (STIs) also increases vulnerability to syphilis, as the presence of one STI can facilitate the transmission of others. Risk reduction strategies include consistent use of barrier protection methods like condoms, regular STI screening, and prompt treatment of infected partners. Pregnant women should undergo routine syphilis screening during pregnancy to prevent congenital infection. Public health initiatives aimed at education, screening, and contact tracing are vital for controlling the spread of syphilis and safeguarding community health.
Final Thoughts: Importance of Awareness and Early Intervention Syphilis, despite being treatable and curable, remains a public health challenge due to its often subtle and asymptomatic nature in the early stages. Increased awareness, regular screening, and prompt treatment are essential components in controlling its spread. Individuals engaging in high-risk behaviors should prioritize testing and consult healthcare providers if any signs or symptoms appear. With early diagnosis and proper treatment, syphilis can be effectively managed, preventing long-term complications and reducing transmission rates. Education and awareness campaigns are key to combating this re-emerging infection and protecting community health for the future.