A Comprehensive Guide to Perioral Dermatitis: Symptoms, Causes, and Treatment Strategies
Perioral dermatitis is a chronic skin condition characterized by redness and bumps around the mouth, often mistaken for acne. This comprehensive guide explores its symptoms, causes, and effective treatment options. Understanding triggers such as corticosteroid use, hormonal shifts, and environmental factors is vital for management. The article emphasizes lifestyle modifications, proper skincare routines, and medical therapies like topical and oral antibiotics for successful treatment. Prevention strategies include avoiding irritants, using gentle skincare products, and protecting skin from sun damage. With proper care, most patients can achieve significant symptom relief and healthier skin.

Understanding Perioral Dermatitis: Symptoms, Causes, and Effective Management
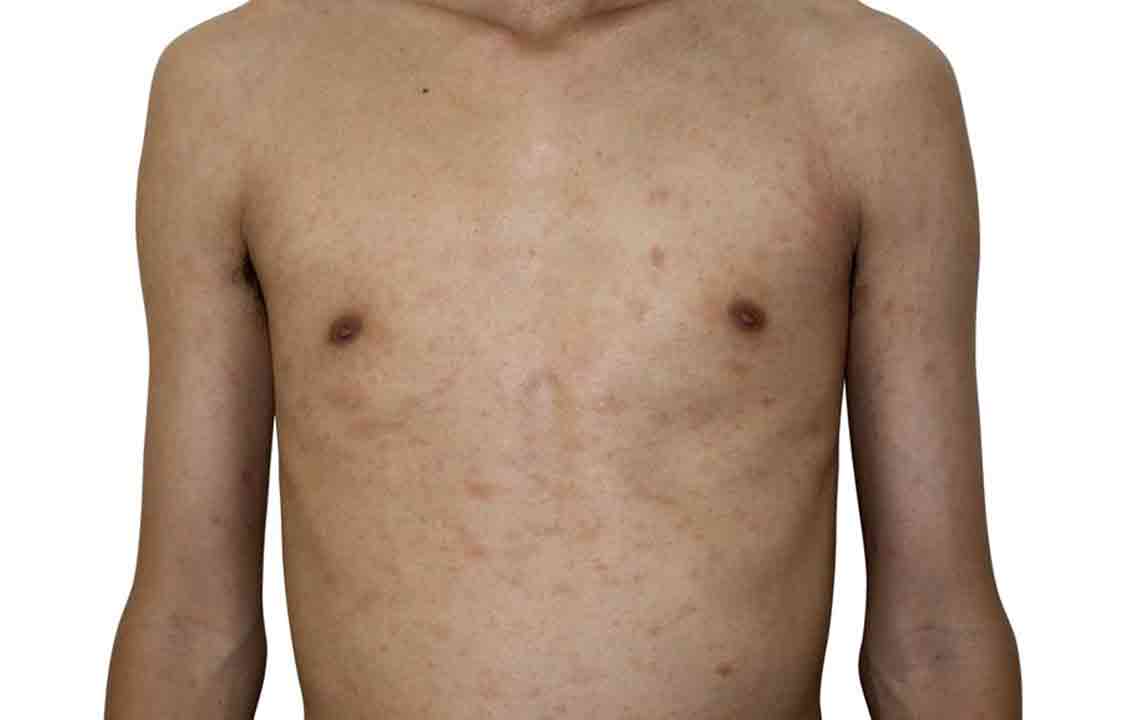
Perioral dermatitis is a common yet often misunderstood skin condition characterized by redness, inflammation, and irritation around the mouth area. This dermatological issue can last for extended periods, ranging from a few weeks to several months or even years if not correctly addressed. It can also affect neighboring regions such as the nose and eyes, leading to a condition known as periorificial dermatitis. Due to its appearance, perioral dermatitis is frequently misdiagnosed as acne, but it differs in terms of symptoms, causes, and treatment approaches.
Perioral dermatitis manifests primarily through small, red, sometimes pus-filled bumps clustered around the mouth, chin, and sometimes along the nose or eyes. These bumps can be accompanied by symptoms such as itching, burning sensations, and flaky, dry skin patches. The discomfort and aesthetic concerns make it a distressing condition, affecting a person's confidence and daily life. Identifying the correct diagnosis is crucial since treatments for acne or other dermatological conditions may not be effective, or could even exacerbate perioral dermatitis.
Understanding the Causes of Perioral Dermatitis
Multiple factors can contribute to the development of perioral dermatitis. The most common causes include the long-term usage of topical corticosteroids and other skincare products. Overuse of potent creams or harsh cosmetics that contain irritants like parabens, fragrances, or alcohol can weaken the skin barrier, making it more susceptible to inflammation. Hormonal fluctuations, particularly in women during certain phases of their menstrual cycle, pregnancy, or menopause, can also trigger or worsen this condition.
Immune system dysfunctions or sensitivities may predispose individuals to developing perioral dermatitis. Environmental influences such as exposure to ultraviolet (UV) rays from the sun are also significant contributors. UV radiation can impair skin integrity and exacerbate inflammation. Additionally, toothpaste containing fluoride has been linked in some cases to worsening peri-oral skin issues, although this varies among individuals.
Diagnosing Perioral Dermatitis
Diagnosis primarily depends on clinical evaluation by a dermatologist. The specialist will examine the affected skin area, noting the characteristic appearance of small red bumps, papules, and possible flaking. Since the symptoms can resemble other skin conditions such as acne, rosacea, or contact dermatitis, a careful history of skincare routines, medication use, and environmental exposures is essential. In some cases, a skin biopsy or patch testing may be conducted to rule out other conditions or identify specific allergens.
Effective Treatment and Management Strategies
Managing perioral dermatitis involves a combination of lifestyle modifications and appropriate medication. The cornerstone of treatment is discontinuing the use of topical corticosteroids, which often worsen or prolong the condition when used long-term. Switching to gentle skincare products devoid of irritants is vital. Incorporating a fragrance-free, non-comedogenic moisturizer can help restore the skin barrier and reduce dryness.
Topical treatments such as metronidazole or erythromycin can be prescribed by dermatologists to reduce inflammation and bacterial overgrowth. In some cases, oral antibiotics like doxycycline or minocycline may be recommended for more severe or persistent cases. Additionally, avoiding triggers like sun exposure by applying broad-spectrum sunscreen and wearing protective clothing is crucial in preventing flare-ups.
Psychological and lifestyle adjustments also play a role in management. Implementing stress-reducing activities, maintaining a consistent skincare routine, and avoiding picking or scratching affected skin can facilitate healing. Regular follow-ups with a dermatologist ensure that treatment plans are adjusted as necessary, fostering better outcomes.
Prevention Tips for Perioral Dermatitis
Preventing perioral dermatitis involves adopting gentle skincare habits and avoiding known irritants. Never overuse corticosteroid creams, and always seek professional advice before starting or stopping any medication. Choose skincare products labeled 'hypoallergenic,' 'fragrance-free,' and 'non-comedogenic.' Regularly apply sunscreen with at least SPF 30 when outdoors to shield the skin from harmful UV rays. Maintaining a healthy diet and managing stress levels can bolster overall skin health. If you notice early signs of skin irritation, consult a dermatologist promptly to prevent progression.
Living with Perioral Dermatitis: Long-Term Outlook
While perioral dermatitis can be persistent and challenging to treat, with proper care and management, most individuals experience significant improvement or complete resolution of symptoms. It is essential to be patient and consistent with prescribed treatments and lifestyle changes. Long-term monitoring ensures that recurrent episodes are kept under control. Educating oneself about triggers and maintaining good skincare hygiene are vital measures for reducing the risk of future flare-ups. With appropriate guidance, many patients can enjoy clearer, healthier skin and improved quality of life.