Comprehensive Guide to Managing and Monitoring Blood Glucose Levels for Optimal Health
This comprehensive guide highlights essential strategies for managing and monitoring blood glucose levels, emphasizing the importance of personalized targets, lifestyle changes, and modern testing methods. It offers practical advice for preventing complications and maintaining overall health through balanced diet, regular exercise, and medical supervision. Empowering readers with knowledge and actionable steps, the article aims to promote better blood sugar control for sustained well-being and disease prevention.

Comprehensive Guide to Managing and Monitoring Blood Glucose Levels for Optimal Health
Blood glucose, also known as blood sugar, is a critical indicator of our metabolic health, serving as the primary source of energy for the body's cells. The levels of glucose in the bloodstream are tightly regulated by insulin, a hormone produced by the pancreas, and the body's ability to process and utilize sugars effectively. Understanding how to monitor and manage blood glucose is essential for preventing lifelong health issues such as diabetes, cardiovascular disease, and other metabolic disorders.
Normal blood glucose levels are measured in milligrams per deciliter (mg/dL). For a healthy individual, fasting blood glucose levels typically range between 70 and 100 mg/dL. After consuming a meal, these levels temporarily increase, reaching up to 120 mg/dL or slightly higher, depending on the meal composition. Regular blood sugar testing helps individuals identify how their body responds to food, exercise, stress, and medication, providing vital information to maintain optimal health.
Blood glucose testing primarily involves fasting blood tests, which are performed after abstaining from eating for at least 8 hours, and postprandial tests conducted after meals. Maintaining blood glucose within the recommended range is critical because persistent high levels (hyperglycemia) can damage blood vessels and nerves, leading to long-term complications such as kidney disease, blindness, and cardiovascular problems. Conversely, low blood sugar levels (hypoglycemia) can cause symptoms like dizziness, sweating, confusion, and in severe cases, loss of consciousness.
To effectively manage blood glucose levels, individuals must adopt a comprehensive approach that includes dietary modifications, physical activity, diligent monitoring, and, if necessary, medication. Personalized blood sugar targets are essential, as they account for age, overall health, and specific medical conditions. For most non-diabetic individuals, maintaining fasting blood sugar under 100 mg/dL and post-meal levels below 140 mg/dL is desirable. However, these targets may vary for people with diabetes, often starting with higher initial goals to prevent hypoglycemia and gradually tightening control over time.
Diet plays a vital role in regulating blood glucose. Consuming a balanced diet rich in fiber, lean proteins, healthy fats, and whole grains helps slow carbohydrate absorption, preventing spikes in blood sugar. Limiting processed sugars, sugary drinks, and refined carbohydrates is equally important. Regular physical activity enhances insulin sensitivity, allowing muscles to use glucose more efficiently. Even moderate activities such as brisk walking, cycling, or yoga can significantly improve glucose control.
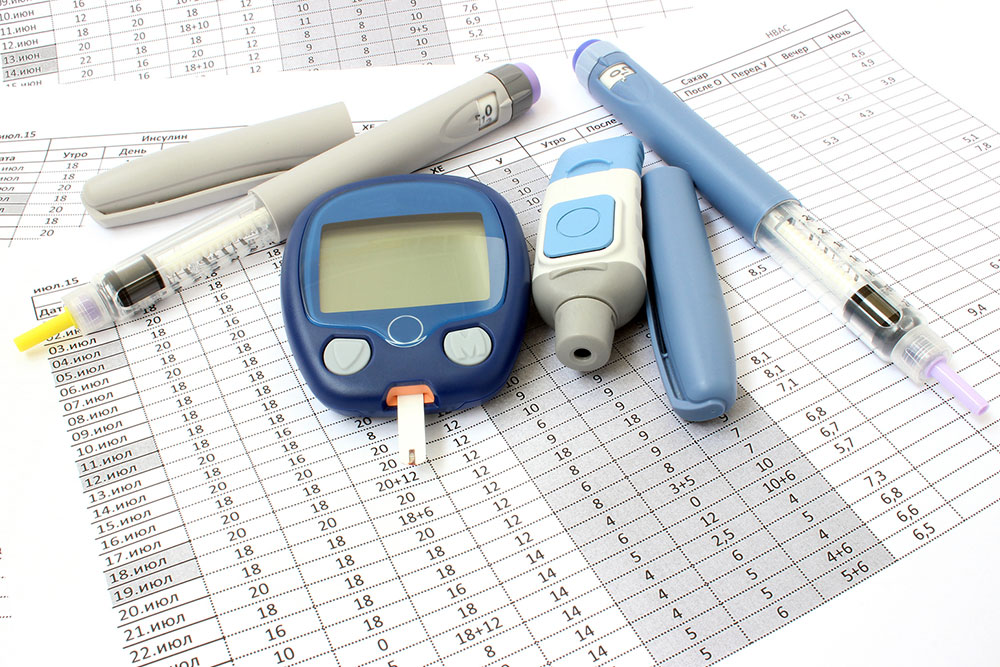
Monitoring blood glucose levels routinely allows individuals and healthcare providers to detect abnormal trends early and adjust management strategies accordingly. Techniques such as fingerstick blood testing using glucometers or continuous glucose monitoring (CGM) devices provide real-time insights into blood sugar fluctuations throughout the day. These tools help in identifying patterns, managing hypoglycemia episodes, and optimizing medication doses.
For individuals diagnosed with diabetes, establishing personalized goals is vital. Healthcare professionals often recommend fasting blood sugar levels between 80 and 130 mg/dL and post-meal levels below 180 mg/dL, but these targets can vary. Adherence to medication regimens, lifestyle adjustments, and consistent monitoring are critical components of management plans. Moreover, education about recognizing symptoms of hypo- or hyperglycemia empowers patients to respond promptly, reducing health risks.
In addition to lifestyle interventions, ongoing medical supervision ensures timely adjustments to treatment plans, minimizing complications. Regular check-ups with healthcare providers, annual HbA1c testing (which reflects average blood glucose over three months), and screening for diabetes-related complications help maintain optimal health. The goal is to strike a balance that promotes stability in blood sugar levels, prevents acute episodes, and minimizes long-term damage.
In conclusion, managing blood glucose effectively is a cornerstone of metabolic health. By understanding normal ranges, adopting healthy eating habits, maintaining an active lifestyle, and utilizing modern monitoring technologies, individuals can achieve and sustain desired blood sugar levels. Such efforts not only improve current well-being but also significantly reduce the risk of chronic diseases associated with blood glucose dysregulation. Empowered with knowledge and supported by medical guidance, anyone can take proactive steps toward better blood sugar control and overall health longevity.
Effective blood glucose management involves understanding normal ranges, monitoring regularly, and making lifestyle modifications. Personalized dietary plans, physical activity, and medical supervision are critical to preventing and controlling diabetes-related complications. Modern tools like continuous glucose monitors enhance real-time tracking, allowing proactive adjustments for healthier outcomes. Consistent efforts in managing blood sugar levels promote long-term health and disease prevention, empowering individuals to lead healthier lives through informed choices and professional guidance.