Comprehensive Strategies for Managing Diverticulitis: Prevention, Treatment, and Recovery
This comprehensive article explores effective management strategies for diverticulitis, covering causes, symptoms, conservative treatments, surgical options, and preventive measures. It provides valuable insights into how patients can navigate treatment and reduce recurrence risks through lifestyle adjustments and medical care. Designed for patients and healthcare providers alike, this guide emphasizes early diagnosis, personalized treatment plans, and preventive habits to manage this widespread gastrointestinal condition effectively.
In-Depth Guide to Effectively Handling Diverticulitis
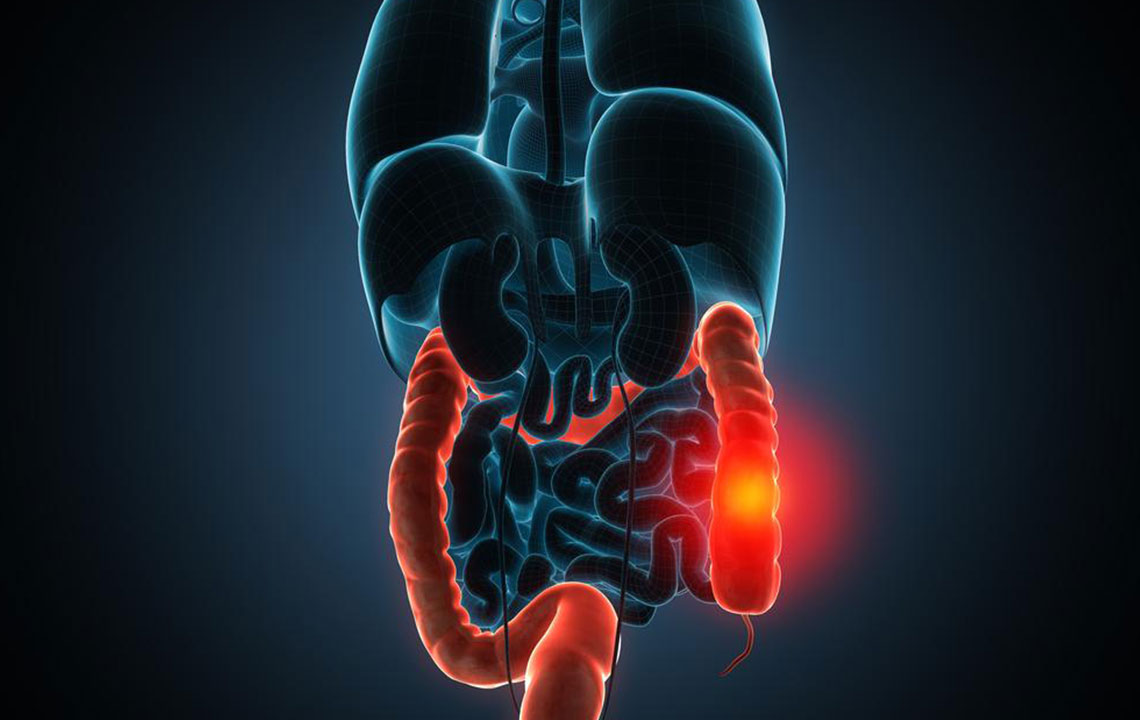
Diverticulitis, a prevalent gastrointestinal condition, affects a significant portion of the adult population worldwide, especially those over the age of 50. It involves inflammation or infection of small pouches known as diverticula that form in the walls of the colon. While many individuals with diverticulosis (presence of diverticula) remain symptom-free, any complication involving inflammation turns the condition into diverticulitis, which can vary from mild discomfort to severe health emergencies. Understanding the causes, symptoms, and comprehensive management techniques is crucial for effective treatment and prevention.
Diverticulitis develops when diverticula, which are small, bulging pouches in the intestinal lining, become inflamed or infected. The leading risk factors include a low-fiber diet, aging, obesity, lack of physical activity, smoking, and certain medications that weaken colon walls. Dietary habits play a significant role—specifically, diets low in fiber increase the pressure within the colon, causing the intestinal wall to weaken and form diverticula. These pouch-like structures can trap bacteria and waste, leading to inflammation, infection, and subsequent complications.
Understanding the clinical presentation of diverticulitis is essential for prompt diagnosis and treatment. Symptoms can range from mild to severe and often include lower abdominal pain, commonly in the left lower quadrant, tenderness upon touch, and cramping. Patients may also experience changes in bowel habits, such as diarrhea or constipation. Systemic symptoms like fever, chills, malaise, bloating, nausea, and loss of appetite frequently accompany the condition, especially in more severe cases. Recognizing these signs early facilitates timely medical intervention, reducing the risk of complications such as perforation, abscess formation, or fistula development.
Persistent lower abdominal pain and tenderness
Altered bowel patterns—diarrhea or constipation
Fever, chills, and chills
Abdominal bloating, nausea, and decreased appetite
Gas, discomfort, and cramping
Management of diverticulitis hinges on the severity of the presentation. Mild cases are often treated conservatively with supportive measures, including pain control, dietary modifications, and antibiotics if infection is suspected. A diet rich in fiber is generally recommended post-recovery to promote healthy bowel movements and prevent recurrence. Patients are advised to start with a liquid or low-residue diet during the acute phase and gradually transition back to fiber-rich foods as symptoms improve.
For moderate to severe cases, hospitalization may be necessary, particularly if signs of perforation, abscess, or sepsis develop. In such instances, intravenous antibiotics, fluids, and bowel rest are implemented to manage infection and inflammation. Diagnostic imaging, such as CT scans, plays a vital role in assessing the extent of the disease and guiding treatment decisions.
In cases resistant to conservative management or with recurrent episodes, surgical intervention might be required. The most common surgery involves resection of the affected colon segment to remove diseased tissue. In some situations, creating a temporary or permanent colostomy may be necessary to divert fecal flow and allow healing. Advances in minimally invasive techniques, like laparoscopic surgery, have reduced recovery times and postoperative discomfort.
Postoperative care includes follow-up colonoscopy to monitor for other potential pathologies, including colorectal cancer or ischemic changes. Long-term management emphasizes lifestyle modifications—adopting a high-fiber diet, engaging in regular physical activity, quitting smoking, and managing body weight—to reduce recurrence risk. Patients are also encouraged to seek prompt medical attention if new or worsening symptoms occur, ensuring ongoing health and preventing complications.
Overall, managing diverticulitis requires a multidimensional approach tailored to individual patient needs. Combining medical therapy, dietary management, lifestyle changes, and surgical intervention when necessary results in better outcomes and improved quality of life for affected individuals. Educating patients about the importance of prevention and early signs of complications is fundamental in reducing morbidity associated with this common bowel disorder.