Comprehensive Guide to Diverticulitis: Causes, Symptoms, Diagnosis, and Effective Management
This comprehensive guide offers in-depth insights into diverticulitis, including its causes, symptoms, diagnosis methods, treatment options, and preventive strategies. It highlights the importance of lifestyle changes, dietary management, and timely medical intervention to effectively control and prevent complications associated with diverticulitis, promoting optimal intestinal health for patients at risk.

Comprehensive Guide to Diverticulitis: Causes, Symptoms, Diagnosis, and Effective Management
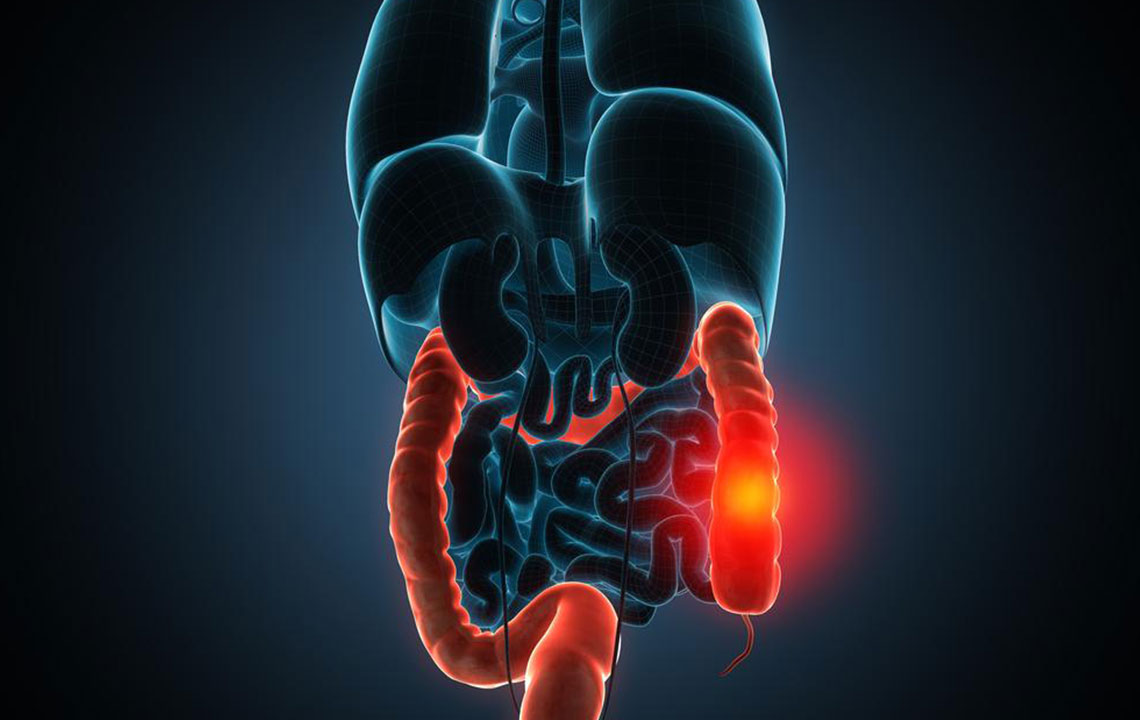
Diverticulitis is a medical condition characterized by the inflammation or infection of small bulging pouches known as diverticula, which develop along the walls of the large intestine, particularly in the colon. While many individuals with diverticulosis remain asymptomatic, the inflammation of these diverticula — termed diverticulitis — can lead to significant health concerns, including severe abdominal pain, bleeding, and potential complications requiring urgent medical attention. Understanding the underlying causes, recognizing the common symptoms, and knowing the available treatment and preventive strategies are crucial for managing this condition effectively. This comprehensive guide is designed to help you gain in-depth knowledge about diverticulitis, empowering you to make informed decisions about your health.
Understanding the Causes of Diverticulitis
Diverticulitis develops primarily when small pouches called diverticula, which form in weak spots of the colon wall, become inflamed or infected. These diverticula are like tiny sacs protruding outward, often forming in areas where blood vessels penetrate the colon wall. The formation of diverticula is a common age-related phenomenon, especially in individuals over 40, though it can occur in younger people too. The exact cause of diverticula formation involves multifactorial processes, including increased pressure within the colon, dietary factors, and lifestyle influences.
Key causes and contributing factors include:
Factors that raise pressure inside the colon, such as chronic constipation, can lead to the development of diverticula. Straining during bowel movements exerts force on the weakened areas of the colon wall, pushing out these pouches.
Dietary Influences: Diets low in fiber and high in refined grains, processed meats, and animal fats can contribute to the development of diverticulosis, which predisposes to diverticulitis. A low-fiber diet leads to harder stools and increased pressure during bowel movements.
Age-Related Changes: As we age, the supporting tissues of the colon weaken, increasing susceptibility to diverticula formation.
Genetics and Family History: A family history of diverticular disease can increase the risk, suggesting a genetic predisposition.
Other Risk Factors: Sedentary lifestyle, obesity, smoking, use of certain medications like NSAIDs, steroids, and blood thinners can also elevate the risk of developing this condition.
When diverticula become inflamed or infected, the condition is termed diverticulitis. This inflammation often leads to more intense symptoms and potential complications such as abscesses, perforations, or fistula formation.
Prevalence and Population at Risk
Diverticulosis is particularly prevalent in Western countries, affecting approximately 50% of individuals over age 60. Its prevalence is on the rise, likely due to dietary changes and aging populations. Men and women are equally affected, and the condition is more common in individuals with a sedentary lifestyle and poor dietary habits.
Recognizing the Symptoms of Diverticulitis
While many individuals with diverticulosis remain symptom-free, diverticulitis manifests through specific symptoms that can vary in intensity. Early recognition of these signs is vital for prompt treatment and to prevent complications.
Common Symptoms
Lower Abdominal Pain: The hallmark symptom is persistent pain in the lower left abdomen. The pain can be sharp, cramping, or steady, often worsening over time. In some cases, especially in younger individuals or those with atypical anatomy, pain may be felt on the right side.
Digestive Discomfort: Symptoms such as bloating, constipation, or, less commonly, diarrhea can accompany the pain.
Nausea and Vomiting: Especially if inflammation affects nearby organs or causes bowel obstruction.
Fever and Chills: Indicative of infection or systemic inflammatory response.
Rectal Bleeding: May occur if inflamed diverticula bleed, leading to bright red blood in stool.
Additional Indicators
Severe complications like abscess formation or perforation can result in symptoms such as sudden, intense abdominal pain, signs of peritonitis (rigid abdomen, fever, tachycardia), and symptoms of sepsis in critical cases.
Diagnosing Diverticulitis: Tests and Procedures
Diagnosis of diverticulitis requires a combination of clinical evaluation and imaging studies. Healthcare providers use various diagnostic tools to confirm inflammation, assess the severity, and rule out other gastrointestinal conditions like appendicitis or inflammatory bowel disease.
Medical History and Physical Examination
The initial assessment includes a detailed medical history focusing on symptoms' duration and severity. Physical examination often reveals tenderness in the lower left abdomen, with possible guarding or rebound tenderness in severe cases.
Laboratory Tests
Complete Blood Count (CBC): Elevated white blood cell count indicating infection.
Inflammatory Markers: Elevated C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) support the presence of inflammation.
Stool Tests: To rule out other causes such as infections or bleeding sources.
Imaging Studies
CT Scan of the Abdomen and Pelvis: The gold standard for diagnosing diverticulitis, revealing inflamed diverticula, abscesses, perforations, or complications.
Abdominal Ultrasound: Useful in certain cases, especially in guiding drainage of abscesses.
Colonoscopy: Typically deferred until symptoms resolve to avoid perforation risk but useful for detecting diverticular disease and ruling out other pathologies.
Managing Diverticulitis: Treatment and Lifestyle Approaches
The management of diverticulitis depends on the severity of the condition, the presence of complications, and the patient's overall health status. Treatment strategies aim to control inflammation, eradicate infection, prevent recurrence, and address complications if they arise.
Conservative Management for Mild Cases
Most uncomplicated diverticulitis cases respond well to outpatient treatment. The key components include:
Dietary Modifications: A period of bowel rest with a liquid or low-fiber diet to reduce colon pressure and allow healing. Once symptoms subside, a gradual transition to a high-fiber diet is recommended to promote regular bowel movements and prevent further episodes.
Medications: Antibiotics are commonly prescribed to treat infection. Pain relievers such as acetaminophen are preferred over NSAIDs, which can increase the risk of gastrointestinal complications.
Hydration: Adequate fluid intake helps soften stool and reduces strain during bowel movements.
Hospitalization and Advanced Interventions
In cases where symptoms are severe, persistent, or complicated by abscesses, fistulas, or perforation, hospitalization may be necessary. Management options include:
Intravenous Antibiotics: Broad-spectrum antibiotics administered in the hospital to control infection.
Drainage of Abscesses: Percutaneous drainage guided by imaging in cases of localized abscesses.
Surgical Intervention: Indicated for perforations, diverticular abscesses unresponsive to drainage, or recurrent episodes. Surgery may involve bowel resection (partial colectomy) or creation of a colostomy.
Surgical Options for Severe or Recurrent Cases
Surgery is considered when conservative measures fail or when there are significant complications. Procedures include:
Bowel Resection (Diverticulectomy): Removal of diseased segments of the colon, often involving sigmoid colectomy.
Colostomy: Creating an opening (stoma) to divert waste if extensive damage or infection is present, which can be reversed in later procedures.
Dietary and Lifestyle Modifications for Prevention
Preventing recurrent diverticulitis episodes involves adopting lifestyle habits that promote proper digestive health:
High-Fiber Diet: Incorporate fruits, vegetables, whole grains, and legumes to ensure regular and soft bowel movements, reducing pressure on the colon.
Hydration: Drink plenty of water daily to assist fiber in softening stool.
Regular Exercise: Physical activity helps maintain healthy bowel function and reduces colonic pressure.
Avoidance of Trigger Foods: Limit intake of processed foods, red meats, and foods high in refined sugars.
No Smoking or Excess Alcohol Consumption: Both can weaken colon tissues and impair healing.
Preventive Tips and When to Seek Medical Help
Early intervention in diverticulitis can prevent serious complications. Seek medical attention if you experience symptoms such as severe abdominal pain, fever, vomiting, rectal bleeding, or signs of peritonitis (rigid abdomen, rapid heartbeat). Regular medical checkups and colon screenings are advisable, especially for individuals over 50 or those with a family history of diverticular disease.
Conclusion
Diverticulitis is a manageable condition with appropriate medical care and lifestyle modifications. Understanding its causes, recognizing early symptoms, and following recommended treatment plans can significantly improve outcomes and prevent future episodes. Maintaining a high-fiber diet, staying hydrated, exercising regularly, and avoiding known risk factors are key steps in promoting long-term colon health. Always consult healthcare professionals for personalized diagnosis and treatment options tailored to your specific condition.