Comprehensive Insights into Osteoporosis: Causes, Types, and Prevention Strategies
This comprehensive article provides an in-depth look at osteoporosis, exploring its causes, types, risk factors, and prevention strategies. It emphasizes the importance of understanding bone remodeling processes and implementing lifestyle modifications and medical treatments to maintain bone health, especially in at-risk populations like postmenopausal women. Early detection and proactive management are key to reducing fracture risk and improving quality of life.

Osteoporosis is a pervasive skeletal disorder characterized by significant loss of bone density and deterioration of bone tissue, which markedly increases the risk of fractures. Often termed a silent disease, osteoporosis progresses subtly and manifests only when a fracture occurs. Gaining an in-depth understanding of its underlying causes is crucial for early prevention, effective management, and improving patients' quality of life. This article delves into the fundamental functions of healthy bones, explores the primary factors contributing to osteoporosis development, examines the various types of the disease, and discusses strategies for prevention and treatment.
Bones are dynamic organs constituting the human skeleton, serving multiple vital roles, from providing structural support and facilitating movement to storing essential minerals such as calcium and phosphorus. These minerals are vital for maintaining bone strength and integrity. Normal bone health is maintained through a continuous process called remodeling, which involves two critical phases: bone resorption and bone formation.
The Process of Bone Remodeling
Bone remodeling is a sophisticated biological mechanism, meticulously balanced to ensure skeletal strength and mineral homeostasis. During resorption, specialized cells known as osteoclasts break down old or damaged bone tissue, releasing calcium and phosphorus back into the bloodstream. Following resorption, osteoblasts—another type of bone cell—are responsible for constructing new bone tissue, depositing minerals onto the existing structure. This process requires adequate intake and availability of calcium and phosphorus, emphasizing the importance of proper nutrition.
When the balance between osteoclast activity and osteoblast activity tilts toward excessive resorption or insufficient formation, bone mass gradually diminishes. Over time, this imbalance leads to the weakening of bones, characteristic of osteoporosis.
Primary vs. Secondary Osteoporosis: Understanding the Differences
Osteoporosis manifests in two main forms—primary and secondary—each with distinct underlying causes and risk factors.
Primary Osteoporosis
Primary osteoporosis is the most common form and predominantly associated with the natural aging process. It is especially prevalent among postmenopausal women due to declining estrogen levels, a hormone critical for maintaining bone density. Estrogen deficiency accelerates osteoclastic activity, leading to increased bone resorption. In addition to age and menopause, lifestyle factors such as poor diet, insufficient physical activity, smoking, excessive alcohol consumption, and genetic predisposition significantly influence the risk of developing primary osteoporosis.
Secondary Osteoporosis
Secondary osteoporosis results from underlying medical conditions or medication use that adversely affect bone metabolism. Medical conditions such as hyperthyroidism, rheumatoid arthritis, chronic kidney disease, celiac disease, and other endocrine disorders disrupt normal bone remodeling processes. Certain medications—most notably glucocorticoids (steroids), anticonvulsants, and some antidepressants—also contribute to decreased bone density. Recognizing secondary causes is essential for targeted treatment, as managing the underlying condition can mitigate bone loss.
Risk Factors and Prevention Strategies
Preventing osteoporosis involves a multifaceted approach focusing on lifestyle modifications, nutritional adequacy, and medical intervention when necessary.
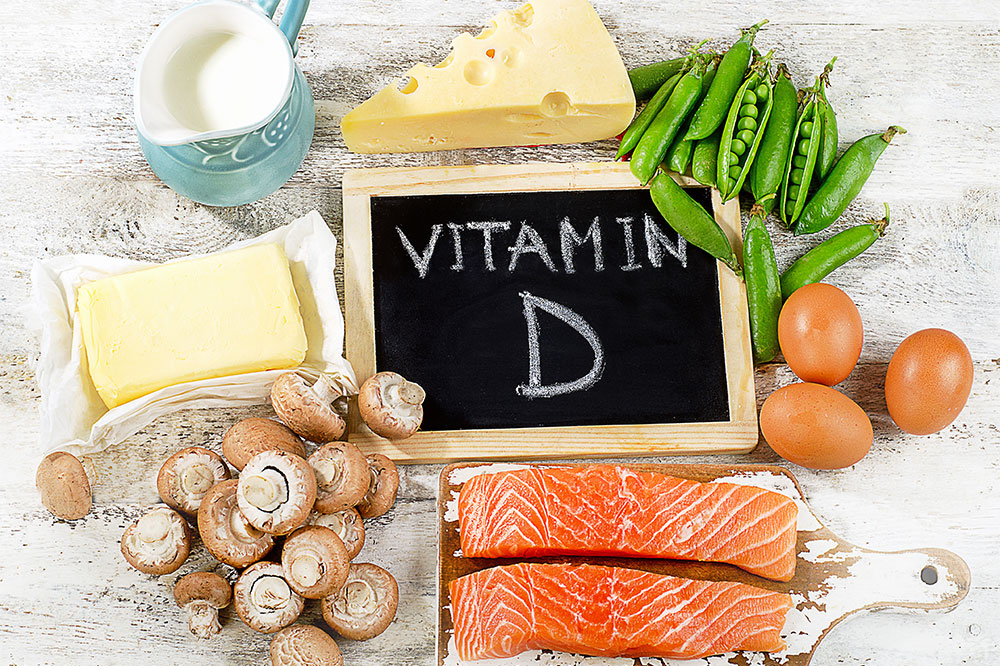
Nutrition: Adequate intake of calcium (usually 1000-1200 mg daily) and vitamin D (600-800 IU daily) is vital for optimal bone health. Dairy products, leafy green vegetables, fortified foods, and supplements are primary sources. Vitamin D facilitates calcium absorption in the gut.
Physical Activity: Weight-bearing and resistance exercises stimulate bone formation and retard bone loss. Regular activities such as walking, jogging, dancing, and strength training are highly beneficial.
Lifestyle Choices: Avoidance of smoking, limiting alcohol consumption, maintaining a healthy weight, and fall prevention measures are critical components.
Medical Evaluation and Treatment: Bone mineral density testing (DEXA scans) helps in early detection. Pharmacological treatments, including bisphosphonates, selective estrogen receptor modulators (SERMs), hormone therapy, and newer agents like denosumab, are used to increase bone density.
Conclusion: The Importance of Early Intervention
Understanding the causes of osteoporosis is fundamental to its prevention and management. Since the disease can silently weaken bones over years, early diagnosis through screening and appropriate lifestyle modifications can significantly reduce fracture risks. With advances in medical science, effective treatments are available to help maintain bone strength and improve quality of life for those affected. Promoting awareness about risk factors and preventive strategies is essential in tackling this widespread health concern.
By adopting a proactive approach, incorporating proper nutrition, engaging in regular physical activity, and seeking timely medical advice, individuals can significantly lower their chances of developing osteoporosis and enjoy healthier, stronger bones throughout their lives.