Comprehensive Guide to Diagnosing and Assessing Chronic Obstructive Pulmonary Disease (COPD)
This comprehensive guide discusses the methods and procedures used to diagnose COPD, including spirometry, imaging, blood tests, and disease staging. It emphasizes the importance of early detection and accurate assessment for effective management of COPD, highlighting key diagnostic criteria and evaluation processes for optimal patient care.

Comprehensive Approach to Diagnosing and Evaluating Chronic Obstructive Pulmonary Disease (COPD)
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disorder that significantly impacts breathing and quality of life. Accurate diagnosis is essential for effective management and treatment planning. The diagnosis of COPD involves a multifaceted approach that includes detailed clinical assessment, advanced pulmonary function testing, laboratory analyses, and imaging studies. Each component plays a crucial role in confirming the presence of COPD, determining its severity, and ruling out other similar respiratory conditions.
Understanding the methods used in diagnosing COPD can help patients recognize the importance of comprehensive evaluation and seek timely medical attention. This in-depth guide will explore the key diagnostic procedures, including spirometry testing, imaging techniques, blood tests, and the staging criteria used by medical professionals to assess disease progression.
The process of diagnosing COPD typically involves several steps:
Assessing clinical symptoms such as chronic cough, sputum production, and shortness of breath
Performing spirometry to quantify lung function
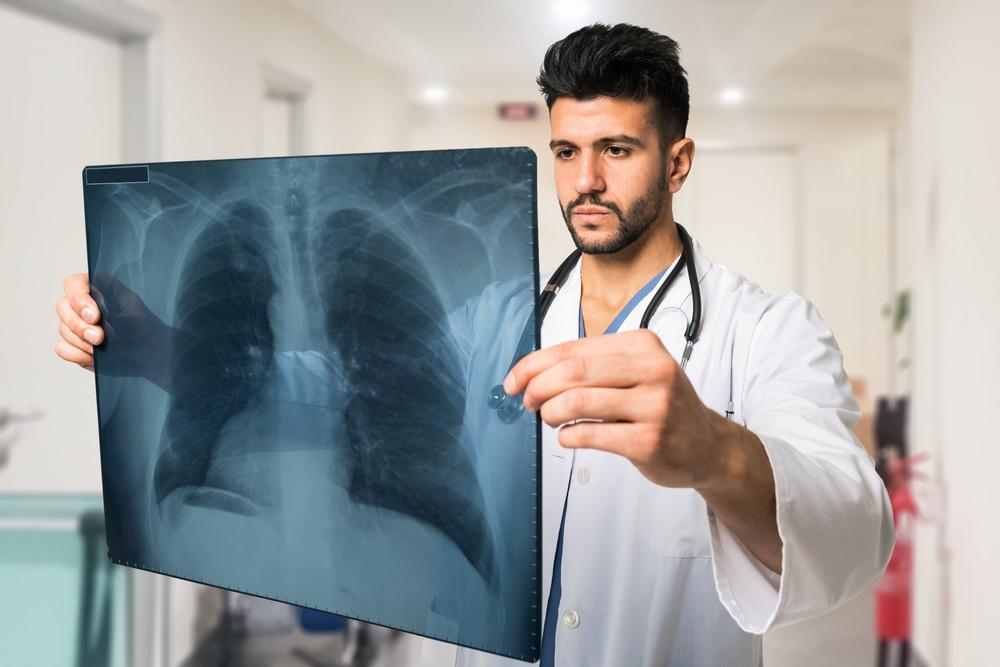
Utilizing imaging studies such as chest X-rays
Conducting laboratory tests to analyze blood and sputum samples
Spirometry: The Cornerstone of COPD Diagnosis
Spirometry remains the most critical diagnostic test for COPD. It evaluates lung function by measuring airflow obstruction. Patients breathe into a device that records various parameters, primarily focusing on the Forced Expiratory Volume in one second (FEV1) and Forced Vital Capacity (FVC). The ratio of FEV1 to FVC (FEV1/FVC) is a vital indicator used to identify airflow limitation characteristic of COPD.
During spirometry, abnormal results can reveal early, even asymptomatic disease, emphasizing the importance of early diagnosis. Typical findings in COPD patients include a reduced FEV1/FVC ratio below 0.7, signifying airflow obstruction, and FEV1 values less than 80% of predicted levels, indicating impaired lung function.
Additional Diagnostic Tools and Tests
Beyond spirometry, several other diagnostic methods help confirm COPD and assess its severity:
Chest X-ray: This imaging technique can sometimes reveal lung hyperinflation and increased radiolucency, indicative of alveolar enlargement and air trapping, common in COPD.
Laboratory Tests: Blood tests may demonstrate elevated red blood cell count as a compensatory response to chronic hypoxia. Sputum analysis helps detect infections or inflammatory processes. Arterial blood gas (ABG) measurements assess levels of oxygen and carbon dioxide in the blood, providing insight into respiratory efficiency.
Staging COPD: Disease Severity According to Clinical Guidelines
Determining the severity of COPD aids in tailoring appropriate treatment strategies. The American Thoracic Society (ATS) classifies COPD into four stages based on FEV1 percentages:
Stage 1: Mild
FEV1 less than 80% of predicted; symptoms may be mild or absent
Stage 2: Moderate
FEV1 between 50% and 80% of predicted; symptoms like persistent cough, sputum production, and shortness of breath during exertion are common
Stage 3: Severe
FEV1 between 30% and 50%; increased respiratory distress and fatigue often seen
Stage 4: Very Severe
FEV1 below 30% or presence of respiratory failure symptoms; significant limitations in daily activities
These staging criteria help clinicians develop personalized treatment plans, monitor disease progression, and improve patient outcomes through targeted interventions.