Comprehensive Guide to Emphysema: Causes, Diagnosis, and Disease Progression
This comprehensive guide explores emphysema's causes, symptoms, diagnostic procedures, and progression stages. Emphysema, a form of COPD, involves alveolar damage and results in breathing difficulties. Early detection and management are crucial for improving patients' quality of life, with emphasis on risk factors like smoking and genetic predispositions. The article provides insights into diagnostic methods, disease stages, and treatment options, highlighting the importance of timely intervention to slow disease progression and enhance respiratory health.

Comprehensive Guide to Emphysema: Causes, Diagnosis, and Disease Progression
Emphysema is a serious chronic lung condition that falls under the larger umbrella of chronic obstructive pulmonary disease (COPD). It is characterized by damage to the alveoli—the tiny air sacs within the lungs responsible for oxygen exchange—leading to significant breathing difficulties. The disease is often grouped with chronic bronchitis due to their common respiratory impacts, but emphysema specifically involves the destruction of alveolar walls, compromising the lungs’ ability to transfer oxygen into the blood and remove carbon dioxide efficiently. This deterioration results in symptoms that gradually worsen over time, affecting quality of life and physical activity levels.
Despite extensive research, there is currently no cure for emphysema. Management strategies primarily aim to alleviate symptoms, slow disease progression, and improve overall respiratory function. The condition progresses through four identifiable stages, from mild to severe, with early diagnosis being crucial for optimizing treatment outcomes and enhancing life expectancy. The rate at which emphysema advances varies broadly among individuals, influenced by factors such as lifestyle, genetics, and environmental exposures.
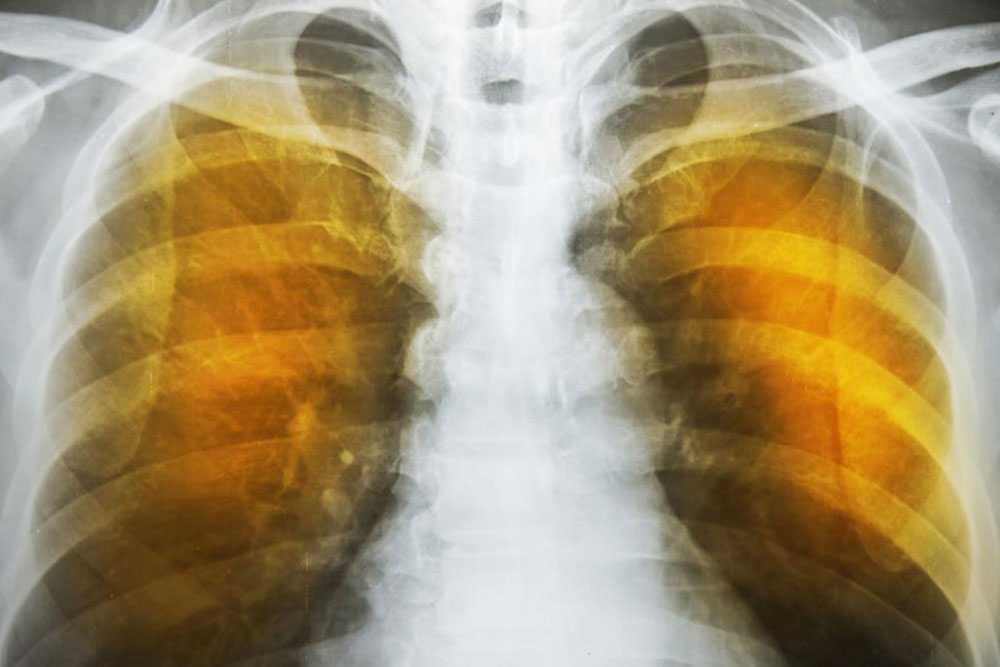
Diagnosis of emphysema involves a combination of imaging, laboratory analyses, and lung function assessments. Imaging modalities like chest X-rays and computed tomography (CT) scans help visualize the extent of lung damage and determine severity. Blood tests evaluate oxygen and carbon dioxide levels in the blood, providing insight into lung efficiency. Lung function tests, especially spirometry, measure airflow, lung capacity, and the ability to expel air forcefully, which are vital for accurate staging.
Understanding the risk factors associated with emphysema is vital for prevention and early detection. The primary risk factor is cigarette smoking—accounting for the majority of cases—due to its irritating and damaging effects on lung tissue. Genetic predispositions, such as alpha-1-antitrypsin deficiency, can increase susceptibility even in non-smokers. Environmental exposures, including prolonged inhalation of pollutants, dust, and chemical fumes, also contribute significantly. Individuals with pre-existing respiratory conditions or frequent respiratory infections are at higher risk for developing emphysema.
Stages of emphysema are typically classified based on the percentage of forced expiratory volume in one second (FEV1), a key metric measured during lung function testing. These stages range from mild (early phase with manageable symptoms) to very severe (significant breathing limitations). The Global Initiative for Chronic Obstructive Lung Disease (GOLD) provides guidelines for staging, which helps tailor treatment plans and predict prognosis. Additionally, composite indexes like BODE (Body mass index, Obstruction, Dyspnea, Exercise capacity) offer comprehensive assessments of disease severity and progression.
Treatment approaches focus on symptom control, preventing further lung damage, and enhancing quality of life. Common interventions include bronchodilators, corticosteroids, pulmonary rehabilitation, and oxygen therapy for advanced stages. Lifestyle modifications such as smoking cessation, avoiding lung irritants, and maintaining a healthy diet are essential. Pulmonary rehabilitation programs combine exercise, education, and behavioral changes to improve respiratory health. While current therapies do not reverse alveolar destruction, early intervention and ongoing management can significantly impact the disease course.
Early detection of emphysema greatly improves treatment effectiveness and can extend survival. Regular screening for at-risk populations, especially smokers or those with genetic predispositions, is recommended. Recognizing early symptoms—such as persistent cough, shortness of breath, and wheezing—enables timely diagnosis and intervention. Monitoring disease progression via FEV1, GOLD, and BODE indexes assists healthcare providers in adjusting treatment regimens and forecasting outcomes. Public awareness campaigns play a critical role in educating individuals about risk factors and the importance of lung health maintenance.
In conclusion, emphysema is a progressive lung disease with significant impacts on breathing and quality of life. While no cure exists, advances in diagnostic techniques and management strategies continue to improve patient outcomes. Prevention through avoiding risk factors like smoking and environmental pollutants remains paramount. Early diagnosis, comprehensive assessment, and personalized treatment plans are essential components of effective disease management. By understanding the causes, diagnosis, and progression of emphysema, patients and healthcare providers can collaborate more effectively to control the disease and improve long-term health prospects.