Understanding the Connection Between Asthma and COPD: Causes, Symptoms, and Treatment Strategies
This comprehensive article explores the critical differences and similarities between asthma and COPD, focusing on their causes, symptoms, and treatment strategies. It highlights the importance of early diagnosis and personalized management to improve patient outcomes. With detailed insights into each condition, the piece aims to enhance understanding of these common respiratory diseases and promote effective care approaches for better quality of life.

Understanding the Connection Between Asthma and COPD: Causes, Symptoms, and Treatment Strategies
Chronic respiratory conditions such as Asthma and Chronic Obstructive Pulmonary Disease (COPD) are prevalent health issues worldwide, often leading to confusion due to their overlapping symptoms and complex clinical features. These respiratory diseases significantly impact patients' quality of life and require tailored management approaches. According to research from the National Heart, Lung, and Blood Institute (NHLBI), approximately 40% of individuals diagnosed with COPD also suffer from asthma, highlighting a substantial overlap between these conditions. In the United States alone, an estimated 24 million people live with COPD, and many are unaware of their condition, underscoring the importance of accurate diagnosis and effective management. This comprehensive review aims to elucidate the similarities and differences between asthma and COPD, exploring their causes, symptoms, diagnostic criteria, and treatment options to promote better understanding and improved patient outcomes.
What Is Asthma? An Overview of the Allergic Respiratory Condition
Asthma is a chronic inflammatory disease of the airways that often begins in childhood but can affect individuals at any age. The exact etiology remains elusive; however, it is widely recognized as an allergic and immune-mediated disorder triggered by environmental allergens and irritants. Common triggers include dust mites, mold spores, pollen, tobacco smoke, air pollution, strong fragrances, certain foods, and chemical additives. Exposure to these allergens leads to airway inflammation, mucous production, and bronchial hyperresponsiveness, resulting in episodes of breathing difficulty. Symptoms of asthma are episodic and can vary in severity—from mild wheezing and cough to severe attacks characterized by difficulty speaking, cyanosis, and respiratory distress. Many patients manage their symptoms effectively through inhaled medications, primarily bronchodilators and corticosteroids, which relax airway muscles and reduce inflammation, respectively.
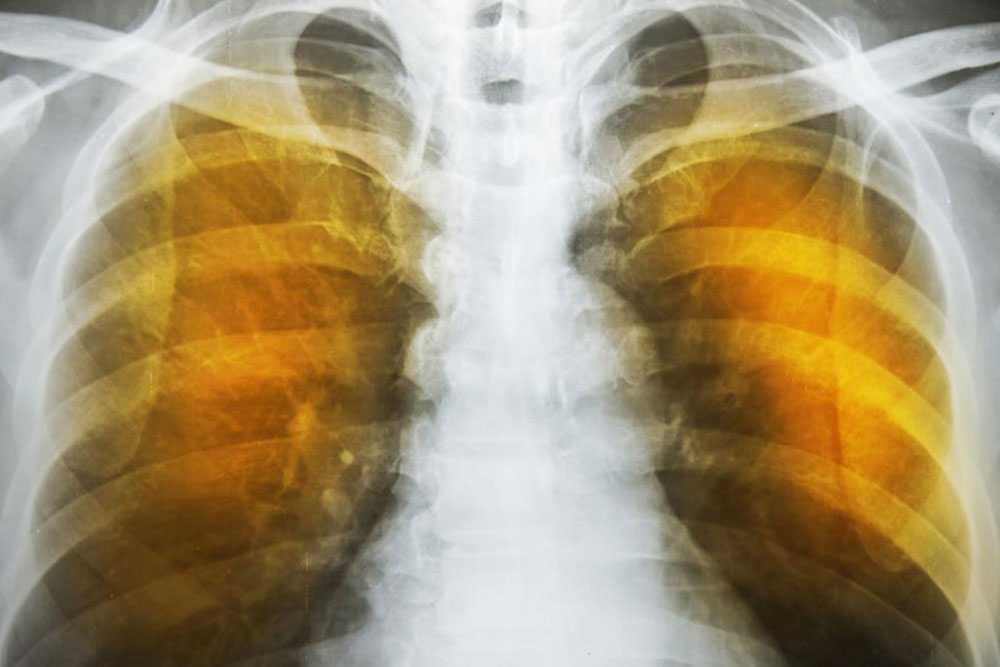
What Is COPD? An Insight into the Progressive Lung Disease
Chronic Obstructive Pulmonary Disease (COPD) predominantly affects middle-aged and older adults and is often linked to long-term exposure to harmful airborne irritants, particularly cigarette smoke. Unlike asthma, COPD is characterized by irreversible damage to the lungs, resulting in a persistent airflow limitation that worsens over time. The disease manifests primarily through symptoms such as a chronic cough, excessive sputum production, and progressive shortness of breath, especially during exertion. Approximately 150,000 Americans succumb to COPD annually, emphasizing its severity and the need for ongoing management. COPD encompasses two main conditions: emphysema and chronic bronchitis. Emphysema involves destruction of alveoli, reducing the lungs’ surface area for gas exchange, while chronic bronchitis is marked by airway inflammation and increased mucus production. Both contribute to airflow obstruction and respiratory compromise.
Causes and Risk Factors of COPD
Unlike asthma, which is primarily allergic in nature, COPD results mainly from external environmental exposures. The primary cause is long-term cigarette smoking, accounting for the majority of cases. Prolonged exposure to other airborne pollutants—including occupational dust, chemical fumes, and indoor/outdoor air pollution—also contributes significantly. Additional risk factors include age (particularly over 40), a history of respiratory infections, and genetic predispositions such as Alpha-1-antitrypsin deficiency—a rare condition that impairs lung tissue protection, increasing vulnerability to damage. Chronic exposure to these irritants leads to sustained inflammation, airway remodeling, and destruction of lung parenchyma, which are hallmarks of COPD progression. Smoking cessation, avoiding environmental pollutants, and early diagnosis are critical steps toward managing and slowing the course of COPD.
Shared Symptoms and Overlaps Between Asthma and COPD
Asthma and COPD, despite their differences, share several clinical features that often lead to diagnostic challenges. Both conditions manifest with symptoms such as shortness of breath, wheezing, chest tightness, and cough. Additionally, they are frequently associated with comorbidities like sinusitis, migraines, hypertension, gastrointestinal ulcers, lung cancer, and reduced mobility. Recognizing these overlapping features is vital for healthcare providers to avoid misdiagnosis and to tailor appropriate treatment plans. For instance, some patients may initially be diagnosed with asthma but later develop COPD symptoms, especially if they have a history of smoking or prolonged exposure to lung irritants. Conversely, some COPD patients may present with asthma-like episodes, complicating the clinical picture.
Approaches to Treatment and Management Strategies
Both asthma and COPD are manageable conditions, but their treatment approaches differ based on their pathophysiology. Asthma is generally considered a reversible airway disease. Its management involves quick-relief inhalers, typically containing short-acting beta-agonists (like albuterol), and long-term control medications such as inhaled corticosteroids, leukotriene modifiers, and biologic therapies for severe cases. Procedures like bronchial thermoplasty—a minimally invasive technique that reduces airway smooth muscle mass—are also available for severe asthma unresponsive to medications. In contrast, COPD involves progressive and irreversible lung damage, making management more about slowing disease progression, relieving symptoms, and preventing exacerbations. Standard treatments include inhaled bronchodilators (long-acting beta-agonists and anticholinergics), inhaled corticosteroids, phosphodiesterase inhibitors, and oxygen therapy in advanced cases. Surgical options like lung volume reduction surgery, bullectomy, and lung transplantation may be considered in severe cases. Pulmonary rehabilitation programs emphasizing exercise training, education, and nutrition are cornerstone therapies to improve quality of life.
The Importance of Early Diagnosis and Personalized Care
Early detection of both asthma and COPD is essential for implementing effective management strategies that can significantly improve patient outcomes. Accurate diagnosis involves comprehensive clinical evaluation, pulmonary function tests, imaging studies, and sometimes allergy testing. Personalized treatment plans tailored to individual disease severity, comorbidities, and lifestyle factors yield the best results. Lifestyle modifications, especially smoking cessation, regular physical activity, and avoidance of triggers, are crucial components of disease management. Healthcare providers often emphasize patient education to enhance understanding of disease processes, medication adherence, and recognition of early exacerbation signs. With proper management, many patients can maintain active, fulfilling lives despite their chronic respiratory conditions.
In conclusion, understanding the nuances of asthma and COPD, their overlapping features, distinct causes, clinical presentations, and treatment options, is vital for effective disease control. While both conditions affect lung function and quality of life, advances in medical therapy and a comprehensive approach to care continue to improve prognosis and daily living for affected individuals.