Comprehensive Guide to Kawasaki Disease: Diagnosis, Symptoms, and Treatment Approaches
Kawasaki disease is a serious condition primarily affecting young children, causing inflammation of blood vessel walls and risking heart complications. Early recognition through symptoms like persistent fever, rash, and redness, coupled with targeted diagnostics such as blood tests and echocardiograms, is vital for effective treatment. Standard care involves immunoglobulin therapy and aspirin to reduce inflammation and prevent coronary artery damage. Prompt medical intervention and ongoing monitoring ensure children recover fully and minimize risks of long-term cardiac issues. This comprehensive guide highlights key diagnosis and treatment strategies for Kawasaki disease.
An In-Depth Look at Kawasaki Disease: Recognizing Symptoms, Diagnostic Procedures, and Effective Treatments
Kawasaki disease, also called mucocutaneous lymph node syndrome, is a serious illness characterized by inflammation of the blood vessel walls throughout the body. This inflammation can obstruct blood flow, especially to the coronary arteries supplying the heart, which may lead to severe cardiovascular complications if left untreated. Although it predominantly affects young children, particularly those under the age of five, early recognition and prompt treatment are crucial in preventing long-term health issues.
In this comprehensive guide, we delve into the detailed aspects of Kawasaki disease, including its symptoms, diagnostic methods, and the most effective treatment strategies. Understanding these components can help caregivers and healthcare providers identify the disease early and manage it effectively to ensure optimal recovery.
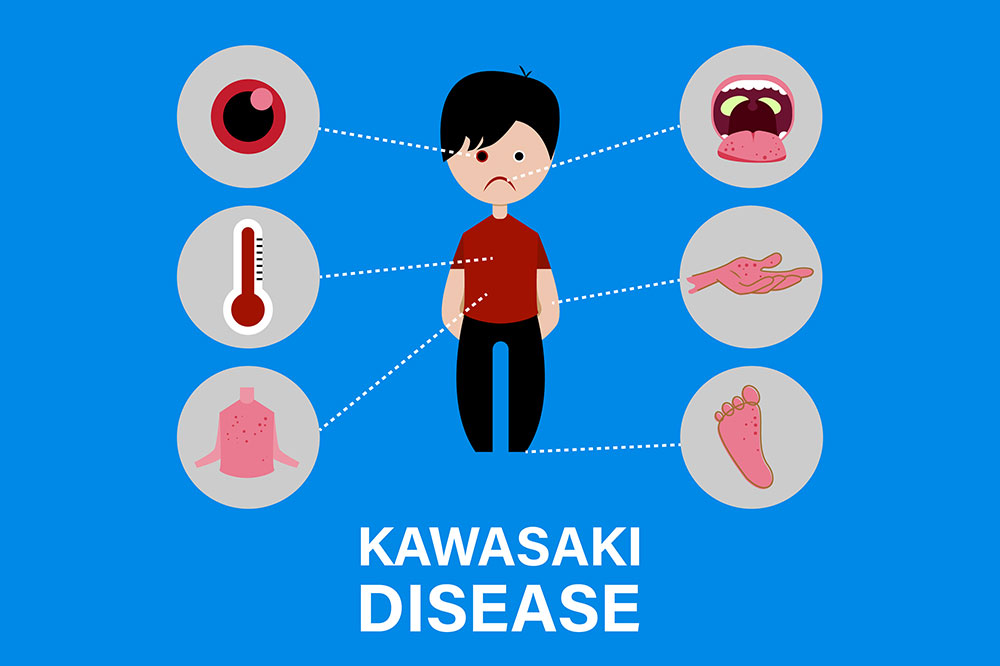
Recognizing the Symptoms of Kawasaki Disease
Early diagnosis starts with awareness of the characteristic symptoms. Children with Kawasaki disease usually present with a persistent high fever lasting more than five days, which does not respond to typical antipypertensive treatments. Along with the fever, other common symptoms include skin redness and rash, swelling of the hands and feet, redness of the eyes (conjunctivitis) without pus, cracked lips, swollen lymph nodes in the neck, and irritation of the mouth and throat.
Additional signs might include irritability, abdominal pain, vomiting, diarrhea, or joint pain. These symptoms can sometimes resemble those of other pediatric illnesses, making it vital for healthcare professionals to perform targeted assessments for an accurate diagnosis.
Diagnostic Procedures for Kawasaki Disease
Since the early symptoms are non-specific, healthcare providers rely on a series of diagnostic tests to distinguish Kawasaki disease from other illnesses like scarlet fever, juvenile rheumatoid arthritis, or other infectious conditions.Key assessments include:
Blood Tests: Blood tests are fundamental in the diagnostic process. They typically reveal elevated white blood cell counts (leukocytosis), increased inflammatory markers like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), and sometimes anemia. In some cases, tests may include measuring B-type natriuretic peptides (BNP), which can indicate cardiac stress but are not solely diagnostic of Kawasaki disease.
Echocardiogram: This ultrasound imaging examines the heart’s structure and function, focusing on the coronary arteries. It is vital for detecting any dilation or aneurysm formation, which are serious complications associated with Kawasaki disease.
Electrocardiogram (ECG): This test records the electrical activity of the heart and helps detect irregular heart rhythms or other cardiac anomalies that might suggest inflammatory damage.
Prompt and accurate diagnosis is key to preventing complications. Healthcare providers synthesize clinical presentation with these test results to confirm Kawasaki disease.
Effective Treatment Strategies for Kawasaki Disease
Once diagnosed, early intervention significantly improves the prognosis. The primary goal of treatment is to reduce fever and inflammation to prevent damage to the coronary arteries.Standard treatment includes high-dose intravenous immunoglobulin (IVIG) administered over a single or multiple doses, which has been shown to rapidly reduce inflammation and lower the risk of coronary artery complications. Aspirin therapy is also commonly prescribed to reduce inflammation and prevent blood clot formation within affected arteries.
Careful monitoring during and after treatment is essential. Children typically undergo repeat echocardiograms and clinical evaluations to track their response and identify any emerging issues.
Long-term management may involve ongoing cardiac evaluations, especially if coronary artery abnormalities are present. In some cases, additional medications or procedures could be necessary to manage these complications effectively.
Understanding the importance of early detection and treatment adherence can make a significant difference in outcomes. Families should maintain regular follow-ups with pediatric cardiologists and healthcare providers to ensure complete recovery and monitor for any potential late-onset complications.
In conclusion, Kawasaki disease, while potentially severe, is highly manageable with prompt diagnosis and appropriate treatment. Increased awareness among caregivers, pediatricians, and health professionals can greatly enhance early detection and improve long-term health prospects for affected children.