Innovative Developments in Oxygen Therapy for Managing Chronic Respiratory Diseases
This comprehensive article explores the latest innovations and technological advancements in oxygen therapy for chronic respiratory conditions like COPD. It covers various delivery systems, monitoring techniques, safety precautions, and future trends, emphasizing improved patient outcomes and safety. Ideal for healthcare providers, patients, and caregivers, the article highlights how modern oxygen therapy enhances quality of life and disease management through personalized treatment protocols and smart technology.

Progressive Strategies and Technological Advances in Oxygen Therapy
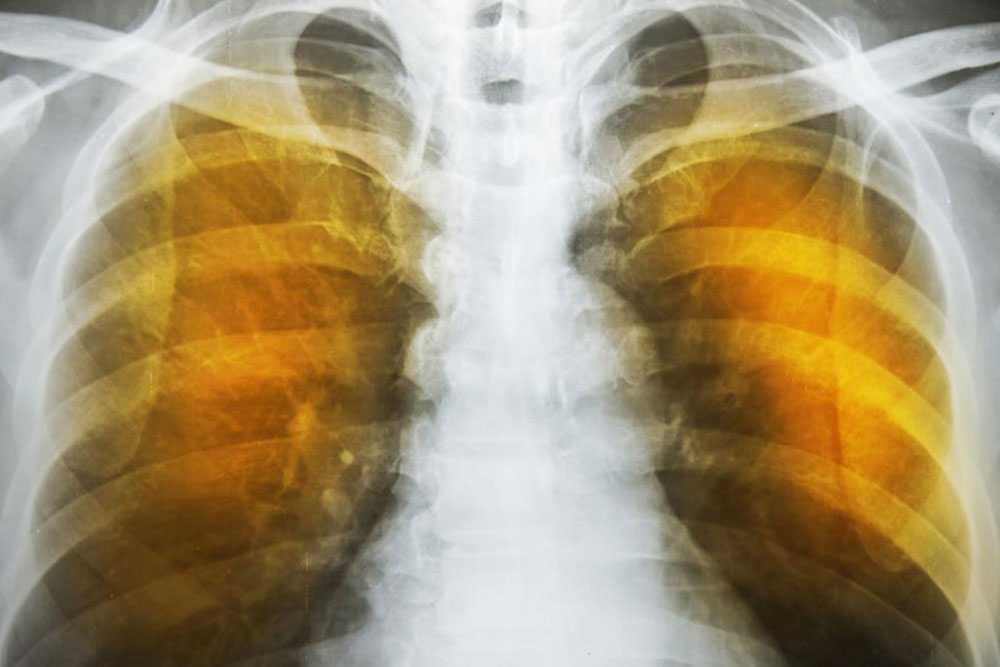
Oxygen therapy has long been a foundational treatment in the management of Chronic Obstructive Pulmonary Disease (COPD) and other chronic respiratory conditions, with a history spanning over sixty years. As medical research has advanced, our understanding of how to best utilize supplemental oxygen has deepened, leading to more sophisticated and personalized treatment approaches. The primary goal remains to improve respiratory function, enhance quality of life, and reduce the risk of severe complications associated with low blood oxygen levels. In recent years, innovations in oxygen delivery systems, monitoring techniques, and treatment protocols have significantly improved patient outcomes, offering greater convenience and safety.
Modern oxygen therapy focuses on delivering oxygen-enriched air efficiently and safely, particularly during physical activity. For patients experiencing activity-induced breathlessness, the use of portable oxygen devices during exercise can markedly improve stamina and overall physical activity levels. This approach not only helps in managing symptoms but also promotes rehabilitation and improves mental well-being by enabling patients to remain active and engaged in daily life activities.
Long-term oxygen therapy (LTOT) is a critical component for individuals with chronic hypoxemia, a condition characterized by consistently low blood oxygen saturation levels. By providing supplemental oxygen over extended periods—often 15 hours or more per day—patients can experience significant improvements in longevity, physical functioning, and overall quality of life. This therapy reduces episodes of breathlessness, decreases the risk of pulmonary hypertension, and prevents the progression of right-sided heart failure, a serious complication associated with COPD. Several delivery systems are utilized in LTOT, including oxygen concentrators, liquid oxygen systems, and traditional compressed oxygen cylinders. Each type offers unique advantages tailored to the patient’s mobility, convenience, and specific needs.
Patients on home oxygen therapy must exercise caution regarding fire safety, as even oxygen levels at 28% can significantly increase the risk of fire hazards. Portable oxygen systems have become increasingly sophisticated, allowing patients to maintain mobility and independence while ensuring safety. These portable units include lightweight cylinders and battery-powered concentrators that facilitate travel and social activities without compromising oxygen delivery.
Achieving optimal blood oxygen saturation—typically between 88% and 92%—is crucial in oxygen therapy. This is accomplished through carefully titrated oxygen flow rates, often administered via nasal cannula at 2-3 liters per minute or through mask adjustments. Continuous monitoring ensures that oxygen delivery is effective without causing hyperoxia or other adverse effects. In acute exacerbations of COPD, recent clinical studies suggest that delivering bronchodilators at flow rates of 6 L/min may enhance therapeutic effectiveness, aiding in rapid symptom relief and stabilization.
Healthcare providers play a vital role in monitoring and adjusting oxygen therapy to prevent complications such as hypercapnia—the buildup of carbon dioxide in the blood—which can occur with excessive oxygen administration. Regular assessments of blood gases, oxygen saturation levels, and patient symptoms are essential to ensure safe and effective treatment. Advances in pulse oximetry and arterial blood gas analysis have facilitated real-time monitoring, enabling more precise control of oxygen delivery tailored to each patient’s condition.
Looking ahead, ongoing research continues to refine oxygen therapy protocols, integrate new technology, and improve patient safety. The development of smart oxygen delivery systems with integrated sensors allows for automatic adjustments based on real-time oxygen saturation readings, significantly reducing the risk of both hypoxia and hyperoxia. Telemedicine approaches also enable remote monitoring and management, providing timely interventions and reducing hospital visits. As our understanding of respiratory pathophysiology evolves, so too will the tools and techniques used in oxygen therapy, making it safer, more effective, and more accessible for patients with chronic respiratory illnesses.