Comprehensive Strategies for Managing Ulcerative Colitis: An In-Depth Guide
Ulcerative colitis is a chronic inflammatory bowel disease impacting many individuals worldwide. This comprehensive guide explores symptoms, diagnosis, and advanced management strategies including medication, diet, and surgery. Lifestyle adjustments and regular medical care are emphasized to help patients effectively control flare-ups, reduce risks, and improve quality of life. Tailored treatments and ongoing support are crucial for long-term health, with recent medical advancements offering new hope for those affected by this challenging condition.

Effective and Holistic Approaches to Ulcerative Colitis Management
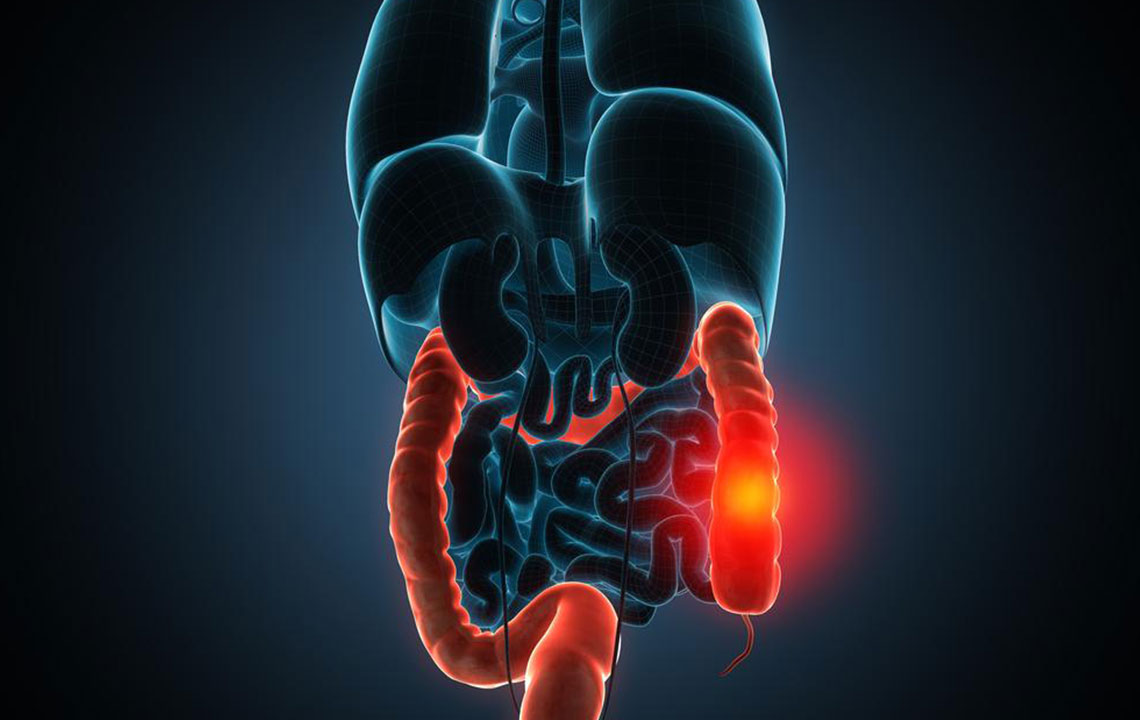
Ulcerative colitis (UC) is a chronic inflammatory condition that primarily affects the large intestine, specifically targeting the innermost lining of the colon and rectum. As a major form of inflammatory bowel disease (IBD), UC presents numerous challenges for those diagnosed, requiring a comprehensive understanding of its causes, symptoms, diagnosis, and treatment options. This article aims to explore all facets of ulcerative colitis management, offering insights into effective strategies that can help patients lead healthier, more comfortable lives.
Ulcerative colitis can strike individuals across various age groups, but it is most commonly diagnosed before the age of 30. The condition’s etiology is believed to involve a complex interplay of genetic susceptibility, immune system irregularities, and environmental triggers. Recognizing early symptoms is crucial for timely diagnosis and effective management.
Understanding the symptoms can facilitate early intervention, which is essential for preventing disease progression and reducing complications.
The demographic most affected by ulcerative colitis includes young adults and teenagers, although it can also occur in older adults. A family history of IBD increases the risk, making genetic predisposition a significant factor in disease development.
Common symptoms associated with UC include:
Persistent abdominal cramps
Severe abdominal pain
Frequent diarrhea episodes
Rectal bleeding and blood in stool
Additional symptoms like fever, fatigue, loss of appetite, and unexplained weight loss can indicate flare-ups or complications. If untreated, persistent inflammation can lead to serious extraintestinal manifestations such as joint pain, eye issues, and liver problems, underscoring the importance of medical attention.
The diagnostic process for ulcerative colitis involves a comprehensive set of examinations including physical assessments, colonoscopy procedures, blood tests, and stool analysis. These diagnostics help distinguish UC from other gastrointestinal conditions such as Crohn’s disease and diverticulitis, ensuring precise treatment approaches.
Long-term, ulcerative colitis increases the risk of developing colon cancer, especially after several years of chronic inflammation. Repeated flare-ups can significantly impair daily functioning and mental health, emphasizing the need for ongoing management and support.
Management of ulcerative colitis revolves around controlling inflammation, reducing flare-ups, and maintaining remission. Treatment strategies are multifaceted, combining pharmacological interventions, lifestyle changes, and sometimes surgical procedures.
Medications such as aminosalicylates, corticosteroids, immunomodulators, and biologics aim to modulate the immune response, decrease inflammation, and promote healing of the intestinal lining. Dietary modifications play a key role in symptom control, with patients encouraged to adopt a balanced, nutrient-rich diet tailored to individual needs.
In severe cases or when medical therapy fails, surgical intervention becomes necessary. Ulcerative colitis surgery typically involves removal of the diseased colon and rectum, with the creation of an internal pouch ( ileal pouch-anal anastomosis ) to restore bowel function and improve quality of life.
Beyond medical treatment, lifestyle choices such as regular exercise, adequate sleep, stress management, and avoiding triggers like smoking or certain foods can reduce the frequency and severity of flare-ups. Early diagnosis and continuous follow-up with healthcare professionals are vital to adapt treatment plans and achieve better health outcomes.
Living with ulcerative colitis requires ongoing effort and support, but with the right strategies, patients can manage symptoms effectively and minimize complications. Advances in medical research continue to improve treatment options, offering hope for enhanced quality of life. Education, lifestyle adjustments, and vigilant medical care are the cornerstones of successful UC management, empowering patients to take control of their health and well-being.