Comprehensive Guide to Ulcerative Colitis: Symptoms, Causes, and Dietary Strategies
Ulcerative colitis is a chronic inflammatory condition of the colon that requires early recognition and proper management. This comprehensive guide discusses symptoms, causes, dietary adjustments, and lifestyle tips to help affected individuals control their symptoms and improve their quality of life through tailored treatments and proactive lifestyle changes.

Comprehensive Guide to Ulcerative Colitis: Symptoms, Causes, and Dietary Strategies
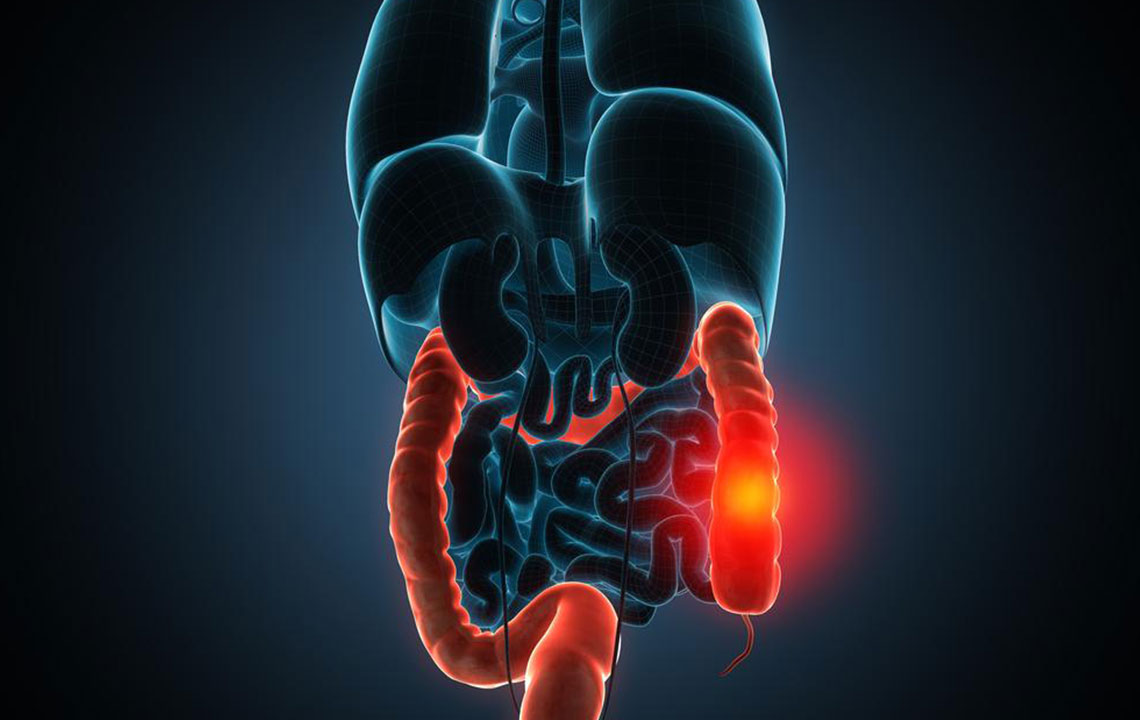
Ulcerative colitis is a persistent, long-term health condition that specifically affects the large intestine, also known as the colon. It is characterized by inflammation, ulcer formation, and irritation of the inner lining of the colon walls. This condition profoundly impacts the quality of life for those affected, especially individuals in their late teens to early thirties. While a definitive cure remains elusive at present, timely diagnosis combined with effective management strategies can significantly control and alleviate the symptoms, enabling patients to lead more comfortable lives. An essential aspect of managing ulcerative colitis involves adopting appropriate dietary habits and seeking professional healthcare guidance to tailor treatments that fit individual needs. Here, we explore the key facets of this condition, including symptoms, causes, dietary recommendations, and lifestyle adjustments.
Recognizing the Symptoms of Ulcerative Colitis
Early detection of ulcerative colitis hinges on awareness of its initial symptoms. The early signs can be subtle and often mistaken for other gastrointestinal issues. Common early symptoms encompass frequent diarrhea, persistent fatigue, unexplained weight loss, abdominal discomfort or cramping, and signs of anemia such as pallor and dizziness. As the disease advances, these symptoms tend to intensify, revealing themselves through blood and mucus in bowel movements, increased urgency, fever, mouth sores, redness in the eyes, and nutritional deficiencies stemming from malabsorption. Children and adolescents may experience delayed growth and development, which underscores the importance of pediatric vigilance. Recognizing these signs early facilitates prompt medical intervention, which is crucial to prevent complications and initiate appropriate treatment plans.
After noticing early symptoms, it becomes imperative to consult healthcare professionals specializing in gastrointestinal disorders. Early diagnosis allows for more targeted management, potentially reducing flare-ups and improving overall health outcomes. Understanding the underlying causes of ulcerative colitis is equally essential in developing effective treatment strategies.
What Causes Ulcerative Colitis?
Despite ongoing research, the precise origin of ulcerative colitis remains somewhat of a mystery. What is known is that the condition involves an abnormal immune response where the immune system mistakenly attacks the colon lining, leading to inflammation and ulceration. Several factors are believed to contribute to this autoimmune reaction. These include environmental triggers, genetic predisposition, and immune system irregularities. Environmental factors such as viral infections, bacterial exposures, and certain antigens can stimulate or exacerbate the condition. Family history significantly increases the risk, indicating a hereditary component. Additionally, immune system disorders that compromise immune regulation can make individuals more susceptible to developing ulcerative colitis. Understanding these risk factors not only aids in early detection but also helps in devising preventative strategies and tailored treatments.
Dietary and Lifestyle Recommendations
Since there is currently no cure for ulcerative colitis, managing symptoms through diet and lifestyle is vital. While no specific diet can eliminate the disease, certain nutritional modifications can mitigate symptoms and promote healing. Patients are advised to avoid foods that commonly trigger flare-ups, including spicy dishes, nuts, seeds, cured meats, raw vegetables, and high-fiber fruits that may irritate the colon. Foods containing sulfur, candies with sorbitol, popcorn, and other processed foods should be limited. Keeping a detailed food diary can help identify individual triggers, allowing for personalized dietary adjustments. Emphasizing foods rich in healthy fats like linoleic acid—found in walnuts, olive oil, and coconut oil—can support intestinal health. Incorporating probiotic-rich foods such as yogurt can help restore gut flora balance. Furthermore, a low FODMAP diet has shown promise in reducing inflammation and symptoms in some patients. Consulting with a registered dietitian ensures that dietary plans are tailored to the individual’s specific needs, disease stage, and treatment goals. In addition to dietary changes, lifestyle modifications such as stress management, regular moderate exercise, and avoiding smoking can have beneficial effects on disease progression and symptom control. Regular medical reviews and adherence to prescribed medication regimens are crucial for optimizing health outcomes.