Comprehensive Guide to Managing Vaginal Atrophy: Symptoms, Causes, and Effective Treatment Strategies
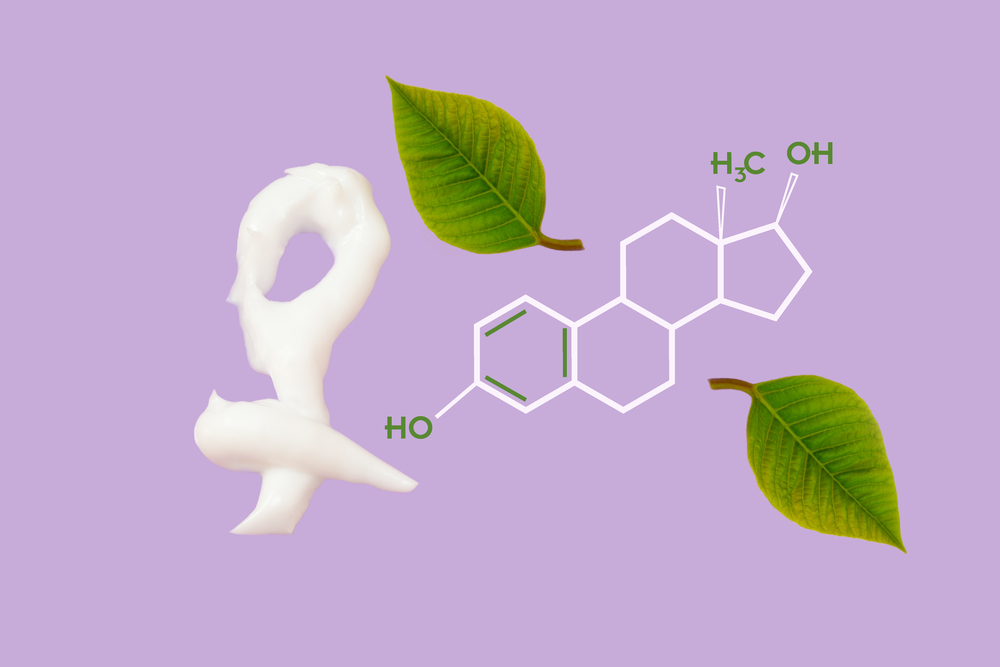
Vaginal atrophy, prevalent among menopausal women, causes discomfort, dryness, and urinary issues. This comprehensive guide covers symptoms, causes, diagnosis, and the latest treatment options, including localized estrogen therapies and lifestyle modifications, to help women effectively manage and improve their quality of life. Early diagnosis and personalized treatment plans are vital for restoring vaginal health and comfort.

Comprehensive Guide to Managing Vaginal Atrophy: Symptoms, Causes, and Effective Treatment Strategies
Understanding Vaginal Atrophy and Its Modern Treatment Options
Vaginal atrophy, also known as genitourinary syndrome of menopause (GSM), is a prevalent condition that primarily affects women during and after menopause. Though commonly associated with aging, it can sometimes occur earlier due to hormonal imbalance or other health factors. This condition results from a significant decline in estrogen levels, which play a crucial role in maintaining the health and integrity of vaginal tissues and surrounding muscles. As estrogen levels decrease, women often experience symptoms such as dryness, thinning of vaginal walls, loss of elasticity, and discomfort, which can considerably impact quality of life.
Beyond discomfort and dryness, vaginal atrophy can lead to more complex issues such as pain during sexual intercourse, urinary tract infections, burning sensations, and in some cases, even bleeding post-intercourse. Due to the intimate nature of these symptoms and their impact on daily life and relationships, addressing vaginal atrophy promptly and effectively is essential for women’s health and well-being.
What Is Vaginal Atrophy?
This condition is predominantly linked to age-related hormonal changes, especially the decline in estrogen levels associated with menopause, but it can also happen at earlier stages due to medical conditions or treatments affecting hormone levels.
The close anatomical and physiological relationship between the urinary and genital systems means that vaginal atrophy often extends its effects to urinary health, leading to issues like burning during urination, urinary urgency, or recurrent urinary infections.
Clinically, vaginal atrophy is characterized by thinning and inflammation of the vaginal walls, loss of lubrication, and reduced elasticity, which collectively contribute to discomfort and increased risk of infections.
Recognizing Common Signs and Symptoms
Women experience diverse symptoms ranging from physical discomfort to urinary symptoms, which include dryness, itching, persistent burning, pain or discomfort during sexual activity, and sometimes light bleeding after intercourse.
Urinary symptoms include burning sensation during urination, increased frequency, urgency, incontinence, and a higher susceptibility to urinary tract infections.
Understanding these symptoms helps in early diagnosis and management to enhance quality of life.
Prevalence and Contributing Risk Factors
Studies reveal that approximately 40-50% of women in the postmenopausal phase experience genitourinary symptoms related to vaginal atrophy, yet many do not seek medical assistance due to embarrassment or lack of awareness.
Major risk factors include smoking, which impairs blood flow and accelerates tissue aging, and certain medical treatments such as chemotherapy, radiation, or hormone suppression therapies.
Conversely, women who have experienced multiple childbirths and maintain active sexual lives tend to have better blood circulation in pelvic tissues, reducing their risk of severe atrophy.
Diagnosis Methods for Vaginal Atrophy
Diagnosis involves comprehensive medical history evaluation, including details of symptoms, sexual activity, and medical background, along with pelvic examinations.
Laboratory tests such as vaginal pH measurement and urine analysis assist in confirming the diagnosis and ruling out infections or other conditions.
Sometimes, tissue biopsies are performed to assess the extent of tissue thinning or inflammation.
Modern Treatment Options for Vaginal Atrophy
While there is no permanent cure for vaginal atrophy, various treatments focus on alleviating symptoms and restoring tissue health, significantly improving quality of life.
Hormone Replacement Therapy (HRT), particularly localized estrogen treatments, remains a highly effective option; however, systemic estrogen therapy is used cautiously due to potential risks.
Vaginal moisturizers and lubricants are popular over-the-counter options that provide immediate symptomatic relief, helping women stay comfortable during daily activities and intimacy.
Among topical treatments, estrogen creams, vaginal suppositories, and vaginal rings deliver targeted hormone therapy directly to the affected tissues, offering sustained relief with minimal systemic absorption.
These localized therapies are generally safe for most women and are recommended after consultation with a healthcare provider to ensure proper usage and monitor for adverse effects.
In addition to hormonal options, lifestyle modifications such as quitting smoking, maintaining a healthy diet, and engaging in pelvic floor exercises can improve overall tissue health and reduce symptoms.
In conclusion, managing vaginal atrophy involves a multi-faceted approach, with tailored treatments based on individual health profiles and symptom severity. Advances in hormone therapy and the availability of effective over-the-counter agents have made it easier for women to regain comfort and confidence in their daily lives. If you experience symptoms of vaginal atrophy, consult a healthcare professional for appropriate diagnosis and personalized treatment options that will help restore vaginal health and improve your overall well-being.