Comprehensive Guide to Vaginal Atrophy: Causes, Symptoms, and Modern Management Strategies
This comprehensive article explores vaginal atrophy, detailing its causes, symptoms, risk factors, diagnostic methods, and current management strategies. It emphasizes the importance of awareness and discusses emerging treatments like SERMs, providing valuable insights for women and healthcare providers seeking effective solutions for GSM.
Comprehensive Guide to Vaginal Atrophy: Causes, Symptoms, and Modern Management Strategies
In-Depth Insights into Vaginal Atrophy and Its Effective Remedies
"Cherish what you have, and continuously seek knowledge and improvement." – Helen Keller
Vaginal atrophy, also known as genitourinary syndrome of menopause (GSM), is a common condition predominantly affecting women after menopause. It is characterized by thinning, dryness, and loss of elasticity in the vaginal walls, often accompanied by urinary tract symptoms. While traditionally believed to occur mainly during menopause due to declining estrogen levels, research indicates that vaginal atrophy can affect women at any age, driven by hormonal fluctuations from menarche onwards. This condition not only affects physical health but can also have profound psychological and emotional impacts, making awareness and management critical.
What Exactly Is Vaginal Atrophy?
This condition involves the thinning of the vaginal lining and a reduction in its elasticity, which plays a vital role in maintaining vaginal health and function.
As the tissue becomes thinner, it leads to decreased moisture production, causing significant discomfort and pain during sexual activity.
Prevalence and Awareness Challenges of GSM
Estimating the exact prevalence is difficult because many women do not seek medical help due to unawareness of the condition or stigma surrounding discussing intimate health issues.
Most women are unaware that their symptoms are linked to hormonal changes associated with aging or other physiological factors.
Recognized Symptoms Linked to Vaginal Atrophy
Primary symptoms include persistent vaginal dryness, burning sensations, itching, unusual vaginal discharge, discomfort during intercourse (dyspareunia), and sometimes light bleeding after sex.
Urinary problems such as painful urination, burning sensations during urination, increased frequency, urgency, and urinary incontinence are also common and are often overlooked parts of the syndrome.
Psychologically, women may experience feelings of unattractiveness, decreased self-esteem, anxiety, and in severe cases, depression, significantly affecting their quality of life.
Factors That Contribute to Higher Risk of Developing Vaginal Atrophy
The primary factor is decreased estrogen levels during and after menopause, which influence the health of vaginal tissues and urinary tract.
Behavioral factors like smoking impair blood circulation and reduce estrogen effectiveness, exacerbating symptoms.
Medications such as hormonal contraceptives and the physiological state of breastfeeding may also influence hormonal balance, affecting vaginal tissue health.
Multiple childbirths via Cesarean section can diminish vaginal blood flow, increasing vulnerability.
Other risk factors include prolonged sexual inactivity, autoimmune conditions like Sjögren’s syndrome, and metabolic disorders such as diabetes, all of which contribute to tissue deterioration.
Diagnostic Approaches for Vaginal Atrophy
Diagnosis is primarily clinical, involving pelvic examination and detailed medical history review to rule out infections or other underlying conditions.
Assessment of urinary symptoms helps differentiate GSM from other urinary tract issues.
Laboratory tests measuring vaginal pH and sampling vaginal fluids help confirm diagnosis and assess the extent of tissue atrophy.
Current Treatment Options and Future Directions
While a definitive cure remains elusive, a variety of treatments help manage and alleviate symptoms effectively.
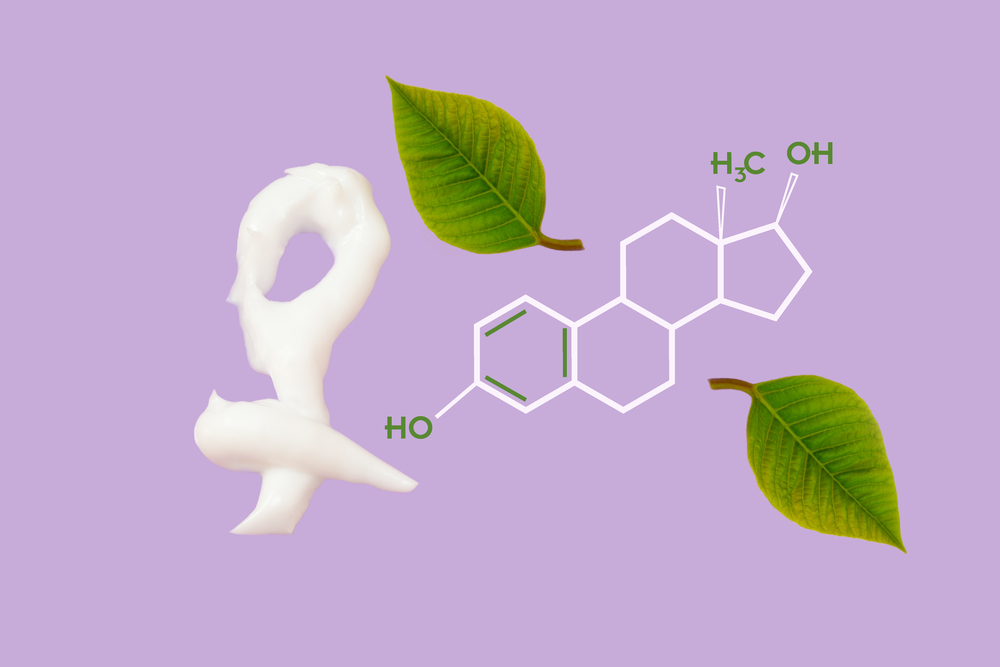
Hormone therapy, particularly topical estrogen applications like creams, rings, or tablets, is widely used but carries systemic absorption risks and is often limited to specific cases.
Vaginal moisturizers and lubricants are commonly recommended for daily use, providing temporary relief from dryness and discomfort. Natural oils, such as coconut or almond oil, are alternative options but should be used cautiously due to potential allergic reactions.
Maintaining regular sexual activity boosts vaginal blood flow and helps in tissue health, serving as a natural therapy.
Emerging therapies include local androgen treatments, with recent studies exploring the role of testosterone and other hormones in improving tissue elasticity and moisture.
Advances in Research: Selective Estrogen Receptor Modulators (SERMs)
Recent scientific investigations focus on SERMs as promising agents capable of providing targeted benefits, such as symptom relief, without systemic estrogen effects.
These tissue-specific agents show potential for treating GSM in women who cannot take traditional hormone therapy due to health risks.
Further research and clinical trials are necessary to establish their safety and efficacy fully, but initial results show encouraging signs.





